In an era where healthcare professionals navigate exponential information growth—with more knowledge generated annually than in all preceding human history—the capacity to systematically capture, organise, and apply information has transformed from advantage to necessity. The modern knowledge worker faces an unprecedented paradox: whilst technology provides access to virtually unlimited information, the human cognitive apparatus remains fundamentally unchanged, constrained by working memory capacity of approximately four discrete elements. Understanding personal knowledge management represents not merely a productivity enhancement, but a cognitive survival strategy for professionals operating within complex, information-intensive environments.
Personal knowledge management transcends simple note-taking or file organisation. Research demonstrates that knowledge workers spend an average of 2.5 hours daily searching for information—representing a 30% productivity loss that costs organisations millions annually. For healthcare professionals managing intricate patient information, evolving research, regulatory requirements, and multidisciplinary collaboration, these inefficiencies compound exponentially. The systematic approach to personal knowledge management addresses this challenge through structured methodologies that transform information chaos into actionable intelligence.
What Constitutes Personal Knowledge Management in Professional Practice?
Personal knowledge management represents a systematic process of collecting, classifying, storing, retrieving, and sharing knowledge that individuals employ throughout their professional activities. Emerging from Frand and Hixon’s 1999 working papers, this discipline addresses the fundamental challenge faced by knowledge workers: responding to information overload through structured systems that convert raw data into actionable knowledge.
The distinction between personal knowledge management and personal information management proves critical. Whilst personal information management focuses predominantly on storage and retrieval mechanisms, understanding personal knowledge management emphasises active engagement with information—the synthesis, connection, and application of knowledge to solve complex problems and generate creative solutions. This distinction becomes particularly relevant in healthcare contexts, where professionals must integrate diverse information sources ranging from peer-reviewed research to patient observations, regulatory guidelines, and interdisciplinary consultations.
The core purpose extends beyond mere organisation. Effective personal knowledge management enables professionals to:
- Externalise cognitive load, freeing mental resources for higher-order thinking
- Create connections between seemingly disparate concepts
- Build cumulative understanding rather than repeatedly relearning information
- Transform consumption into creation through systematic knowledge application
- Develop what cognitive scientists term “distributed cognition”—leveraging tools and systems to extend mental capacity
Research in cognitive science confirms that human short-term memory handles approximately four elements simultaneously. Personal knowledge management systems effectively distribute cognitive burden across external tools, enabling professionals to focus cognitive resources on analysis, synthesis, and application rather than retention and retrieval.
How Do the Four Pillars Support Effective Knowledge Systems?
Understanding personal knowledge management requires mastery of four fundamental pillars that collectively transform information consumption into knowledge creation. These pillars represent sequential yet iterative processes, each building upon the previous whilst informing subsequent activities.
Capture: Systematic Information Collection
The capture pillar encompasses gathering and recording information from diverse sources as it becomes available. Healthcare professionals encounter information through journal articles, conferences, professional discussions, patient interactions, and continuing education—each representing potential knowledge to be systematically captured rather than relying on fallible memory.
Best practice capture mechanisms include digital notebooks with web clipping functionality, voice recording applications for immediate idea capture, and automated collection tools that aggregate information from predetermined sources. The critical principle involves creating frictionless capture systems that integrate seamlessly into existing workflows, minimising resistance to consistent use.
Organise: Structural Knowledge Architecture
Organisation transforms captured information into retrievable knowledge through systematic structuring. This pillar involves breaking information into manageable components and establishing logical relationships that facilitate efficient retrieval. The organisation phase requires developing consistent categorisation schemes—whether through hierarchical folder structures, tagging systems, or network-based linking approaches.
Popular frameworks include the PARA method (Projects, Areas, Resources, Archives), which organises information based on actionability and lifecycle stages, and the Zettelkasten approach, emphasising atomic notes with extensive cross-linking. Healthcare professionals might adapt these frameworks to accommodate clinical specialisations, patient categories, research domains, or professional development areas.
Distil: Extracting Essential Intelligence
Distillation represents the intellectual labour of understanding personal knowledge management—extracting essence from organised information and identifying what proves most relevant. This pillar demands active engagement: summarising in one’s own language, identifying connections between concepts, and integrating new information with existing knowledge structures.
Research demonstrates that active learning retains 93.5% of material after one month, compared to 79% retention from passive learning approaches. The distillation process embodies this active engagement, requiring professionals to synthesise information rather than merely store it, thereby strengthening understanding through cognitive processing.
Express: Transforming Knowledge into Outputs
The expression pillar validates whether knowledge has genuinely been internalised by creating tangible outputs. These outputs might include clinical protocols, educational presentations, research contributions, problem solutions, or shared expertise that benefits colleagues and patients. Expression creates feedback loops that reveal gaps in understanding, reinforce learning through teaching, and demonstrate practical application of accumulated knowledge.
For healthcare professionals, expression might manifest as case study analyses, protocol refinements based on accumulated insights, mentorship of junior colleagues drawing from systematised experience, or contributions to professional discourse informed by comprehensive knowledge synthesis.
Which Maturity Levels Define Personal Knowledge Management Evolution?
Understanding personal knowledge management progression reveals predictable developmental stages, each characterised by distinct capabilities and outcomes. This maturity framework enables professionals to assess current capabilities whilst identifying development pathways.
| Maturity Level | Characteristics | Primary Outcomes | System Sophistication |
|---|---|---|---|
| Level 1: Information Storage | Basic organisation tools; scattered information; heavy memory reliance | Frequent rework; uncertain retrieval | Minimal structure; default configurations |
| Level 2: Managing Knowledge | Regular capture from multiple sources; emerging connections; thought partnership | Reduced cognitive load; improved retention | Systematic capture; consistent organisation |
| Level 3: Enabling Action | Selective information intake; ambitious project execution; knowledge sharing | Enhanced problem-solving; reputation building | Integrated workflows; sophisticated linking |
| Level 4: Personal Knowledge Mastery | Seamless tool integration; continuous output; complete system coherence | Innovation leadership; creative flow state | Holistic ecosystem; automated processes |
This progression from passive information storage to active knowledge mastery typically unfolds over years, requiring consistent practice, regular refinement, and sustained commitment. Healthcare professionals often experience accelerated progression due to inherent information intensity within clinical practice, provided systematic approaches replace ad hoc methods.
The transition between levels represents qualitative shifts in capability. Level 1 practitioners frequently experience information overwhelm and productivity losses from searching and rework. Level 2 practitioners achieve stability and confidence through reliable systems. Level 3 practitioners leverage knowledge for ambitious outcomes and professional advancement. Level 4 practitioners achieve what cognitive psychologists term “flow”—seamless integration where system and user function as unified whole.
What Frameworks Guide Personal Knowledge Management Implementation?
Several established frameworks provide structural guidance for implementing personal knowledge management systems, each emphasising different organisational philosophies whilst sharing common principles.
The Zettelkasten Method
Originating from German scholar Niklas Luhmann’s extensive note system, the Zettelkasten method emphasises atomic notes—each focusing on a single concept—extensively cross-linked to create organic knowledge networks. This approach proves particularly valuable for research-intensive roles where complex theoretical relationships require explicit mapping.
Implementation involves creating fleeting notes during initial encounters, converting these into permanent notes through synthesis and personal interpretation, and developing index notes that provide thematic entry points into the knowledge network. The extensive linking creates emergent insights as connections reveal unexpected relationships between concepts.
The PARA Method
Thiago Forte’s PARA method provides intuitive structure through four categories: Projects (short-term goals with deadlines), Areas (ongoing responsibilities), Resources (topics of interest), and Archives (inactive items). This framework excels for professionals managing multiple concurrent responsibilities whilst maintaining long-term knowledge development.
Healthcare professionals might establish Projects for current patient cohorts or research initiatives, Areas for clinical specialisations and professional development, Resources for continuing education materials and reference databases, and Archives for completed cases and historical documentation.
Digital Mind Gardens
The mind garden metaphor reconceptualises knowledge systems as living, evolving ecosystems rather than static repositories. This approach expects continuous cultivation: adding new information, pruning outdated material, connecting emerging relationships, and allowing organic growth patterns to emerge.
This framework particularly suits professionals in rapidly evolving fields where knowledge currency proves critical. Rather than pursuing comprehensive completeness, mind gardens emphasise relevant cultivation—developing knowledge areas that serve current and anticipated needs whilst allowing natural evolution.
How Do Critical Success Factors Determine System Effectiveness?
Understanding personal knowledge management implementation reveals several critical success factors that differentiate functional systems from abandoned initiatives.
Goal Clarity and Purpose Alignment
Without explicit objectives, knowledge management systems devolve into unfocused accumulation. Research consistently identifies goal clarity as the foundational prerequisite before selecting tools or methodologies. Healthcare professionals must articulate specific problems their system addresses: managing patient information continuity, tracking research developments, supporting evidence-based practice, or facilitating interdisciplinary collaboration.
Consistency and Habit Development
Hermann Ebbinghaus’s forgetting curve research demonstrates that without reinforcement, retention decreases to 21% after 31 days. Regular engagement with knowledge systems—ideally brief daily interactions rather than sporadic intensive sessions—combats this natural decay whilst strengthening neural pathways through spaced repetition.
Research indicates that spaced practice improves retention by 35%, whilst regular review prevents the dramatic decline Ebbinghaus documented. For time-constrained healthcare professionals, establishing modest but consistent engagement patterns (5-10 minutes daily) yields superior outcomes compared to intermittent marathon sessions.
Simplicity and Pragmatism
Complexity represents the primary cause of personal knowledge management failure. The “keep it simple” principle proves crucial—starting with minimal viable systems and adding complexity only when clearly justified by specific needs. Research demonstrates that attempting to implement multiple complex systems simultaneously virtually guarantees abandonment.
Healthcare professionals should resist “shiny object syndrome”—perpetually seeking ideal tools whilst neglecting system use. The optimal system proves to be the one actually employed consistently, not the theoretically superior but practically unused alternative.
Personalisation and Adaptation
No universal personal knowledge management system exists. Effective systems reflect individual learning styles, work contexts, technology preferences, and output goals. Visual learners might emphasise mind mapping and graphical connections; auditory learners might incorporate voice notes and podcast annotations; kinesthetic learners might prioritise hands-on application and teaching others.
Healthcare professionals must adapt frameworks to clinical realities: patient confidentiality requirements, regulatory documentation standards, interdisciplinary communication needs, and evidence-based practice demands. This customisation ensures systems serve actual workflow requirements rather than imposing theoretical ideals disconnected from practice realities.
Why Does Personal Knowledge Management Matter for Healthcare Professionals?
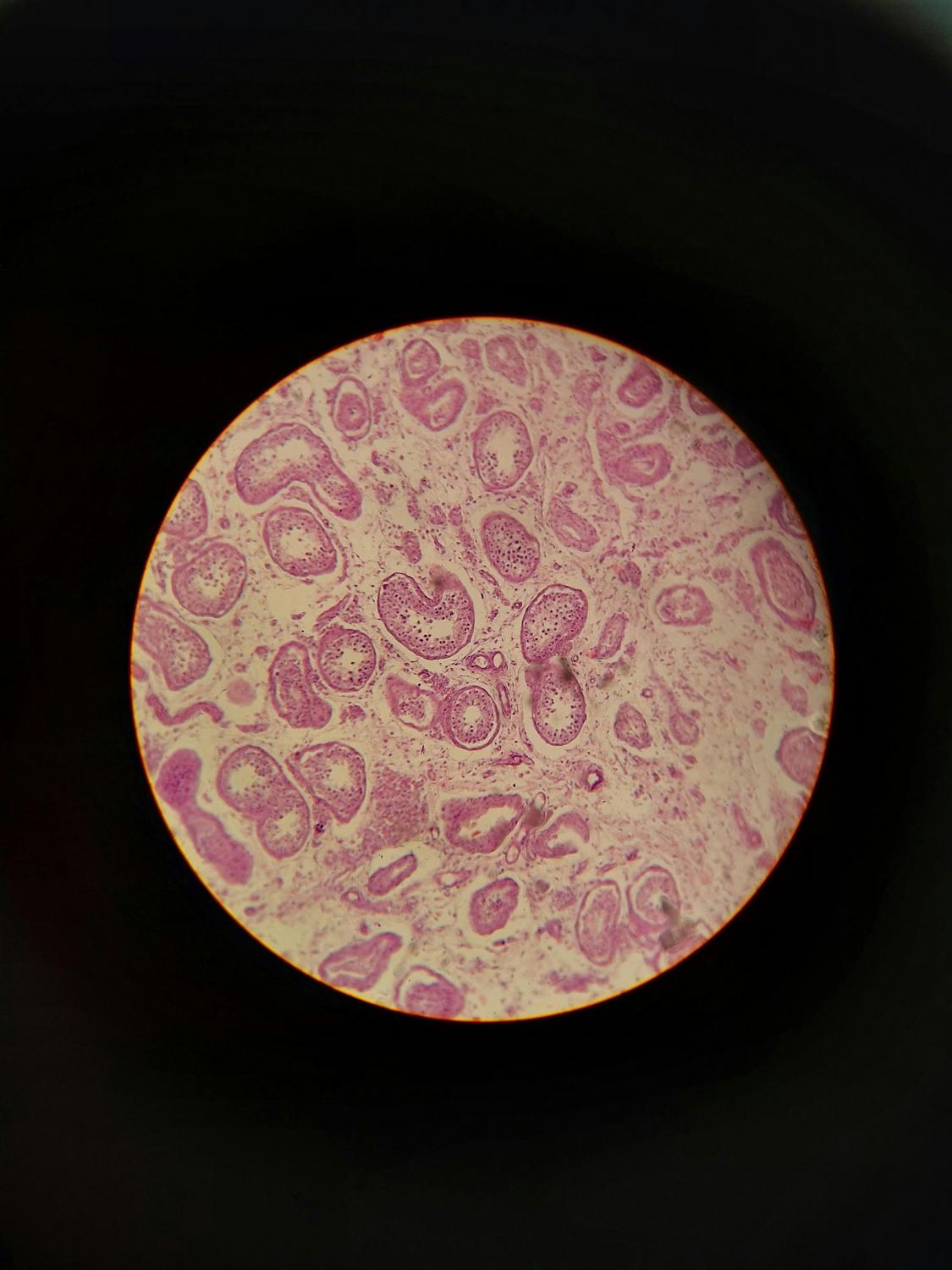
Understanding personal knowledge management assumes particular significance within healthcare contexts where information complexity, regulatory requirements, and patient outcomes create distinctive pressures. Healthcare professionals operate within environments characterised by exponential knowledge growth, multidisciplinary collaboration, continuous professional development mandates, and decision-making with significant consequences.
The wellness connection extends beyond productivity metrics. Research demonstrates that feeling organised and maintaining structured information systems reduces occupational stress, improves decision-making confidence, and supports work-life balance through reduced cognitive load and enhanced efficiency. For healthcare professionals experiencing high burnout rates, these wellness benefits complement professional effectiveness gains.
Organisations with strong knowledge management practices demonstrate 20-25% operational cost reductions, 30% higher revenue growth, and significantly improved employee retention. However, 42% of organisational knowledge dissipates when employees leave—representing substantial loss in healthcare contexts where clinical experience and patient relationship continuity prove invaluable. Effective personal knowledge management systems partially mitigate this loss by externalising tacit knowledge, creating shareable resources, and establishing transferable frameworks.
The cognitive science foundations prove equally compelling. Distributed cognition theory demonstrates that human intelligence extends beyond individual brains to encompass tools, environments, and collaborative systems. Personal knowledge management explicitly leverages this principle, distributing cognitive burden across external systems whilst maintaining human oversight for synthesis, judgement, and application.
Furthermore, continuous learning and mentally stimulating work protect against cognitive decline—the “use it or lose it” hypothesis supported by research on cognitive reserve and aging. Systematic knowledge management inherently promotes continuous learning, intellectual stimulation, and complex problem-solving—activities that preserve cognitive function throughout professional careers.
Implementing Systems Within Professional Healthcare Contexts
Practical implementation requires methodical approaches adapted to healthcare realities. Begin by defining specific purposes: Will the system support patient care continuity? Track professional development? Facilitate research activities? Enable interdisciplinary collaboration? Clear objectives guide subsequent decisions regarding tools, structures, and workflows.
Assess current information ecosystems: Where does critical information currently reside? Which existing tools function effectively? What breaks down under pressure? This assessment reveals integration opportunities and identifies redundant systems that could be consolidated or eliminated.
Choose appropriate tools based on specific requirements rather than general popularity. Consider privacy and confidentiality requirements—particularly relevant in healthcare contexts with stringent patient information protections. Evaluate cross-platform compatibility for professionals working across multiple devices and locations. Prioritise tools offering robust export capabilities to avoid vendor lock-in.
Start focused and small. Select one knowledge domain—perhaps a clinical specialisation or research interest—and develop systematic capture, organisation, and expression practices within that bounded scope. Success builds confidence and reveals refinement opportunities before expanding to additional domains.
Establish review cycles that maintain system currency without consuming excessive time. Weekly reviews process captured information and create connections. Monthly evaluations assess system effectiveness and identify improvements. Quarterly refinements address structural issues. Annual strategic reviews align systems with evolving professional goals.
The integration of artificial intelligence and automation continues accelerating. By 2027, 90% of knowledge management platforms will incorporate generative AI capabilities. Healthcare professionals should anticipate AI-powered recommendations, automated summarisation, intelligent search functionality, and personalised knowledge delivery—whilst maintaining critical evaluation and professional judgement as essential human contributions.
Looking to discuss your health options? Speak to us and see if you’re eligible today.
What distinguishes personal knowledge management from simple note-taking or file organisation?
Understanding personal knowledge management extends beyond passive information storage to encompass active engagement with knowledge through synthesis, connection, and application. Whilst note-taking captures information and file organisation provides retrieval mechanisms, personal knowledge management transforms captured information into actionable intelligence through systematic distillation and expression. The distinction centres on cognitive engagement: personal knowledge management requires actively processing information, identifying relationships, integrating with existing knowledge, and producing tangible outputs that demonstrate genuine understanding rather than mere possession of information.
How much time should healthcare professionals dedicate to maintaining personal knowledge management systems?
Research demonstrates that brief, consistent engagement proves more effective than sporadic intensive sessions. Daily interactions of 5-10 minutes for capturing and processing information, combined with weekly 30-minute reviews for connecting and organising, typically suffice for maintaining functional systems. Monthly evaluations (60-90 minutes) and quarterly refinements (2-3 hours) support system evolution. Critically, effective systems ultimately save substantially more time than they consume—research indicates that organised knowledge workers spend 2.5 fewer hours daily searching for information compared to those with ad hoc approaches, representing net time savings exceeding 10 hours weekly.
Which personal knowledge management tools work best for healthcare professionals managing sensitive information?
Tool selection must prioritise security, privacy, and confidentiality compliance. Local-first applications that store data on controlled devices rather than cloud servers often better satisfy healthcare information protection requirements. Essential features include robust encryption, granular access controls, comprehensive audit trails, and reliable backup mechanisms. Many healthcare organisations mandate specific platforms or provide enterprise systems that satisfy regulatory requirements whilst enabling personal knowledge management functionality. Professionals should prioritise institutional compliance over theoretical tool superiority whilst seeking systems offering sufficient flexibility for personalised workflows within approved frameworks.
Can personal knowledge management systems be implemented alongside existing healthcare documentation requirements?
Effective personal knowledge management complements rather than duplicates mandatory documentation systems. Healthcare professionals might use personal knowledge management for synthesising research relevant to practice, tracking professional development activities, managing interdisciplinary collaboration notes, and developing clinical insights—whilst maintaining separate systems for regulatory-required patient documentation. The key involves identifying knowledge management needs that existing institutional systems inadequately address, then implementing personal solutions for those specific gaps. Integration approaches that connect personal systems with institutional platforms through appropriate interfaces can create synergies whilst maintaining necessary boundaries.
How do personal knowledge management principles apply to interdisciplinary healthcare teams?
Whilst personal knowledge management emphasises individual systems, the principles scale effectively to team contexts. Shared knowledge repositories, collaborative documentation practices, and team-based review cycles adapt personal knowledge management frameworks for collective use. However, successful team knowledge management requires explicit protocols, shared vocabularies, consistent organisational schemes, and designated maintenance responsibilities. Research demonstrates that 54% of organisations employ five or more disconnected knowledge tools, creating fragmentation that undermines effectiveness. Teams should establish unified platforms with agreed structures whilst permitting individual customisation within those frameworks, balancing consistency with personalisation to accommodate diverse working styles and preferences.