In an era where healthcare organisations face unprecedented pressure to deliver exceptional outcomes whilst managing increasingly complex operational demands, the invisible workflows that underpin service delivery often become sources of chaos rather than clarity. Tasks accumulate, bottlenecks emerge, and teams struggle to maintain visibility across fragmented processes. The result? Delayed responses, diminished team morale, and organisational inefficiencies that compound over time. Yet amidst this operational turbulence, a deceptively simple visual management system continues to transform how leading organisations orchestrate their work.
What Is the Kanban Method and Why Does It Matter for Healthcare Organisations?
The Kanban Method represents a visual workflow management system that originated from the Toyota Production System developed by Taiichi Ohno in the 1940s. The term “kanban” derives from the Japanese words “kan” (visual) and “ban” (card or board), literally meaning “visual signal.” What began as a solution to Toyota’s resource constraints—where the company needed to achieve a tenfold productivity increase to compete with American manufacturers—has evolved into a universal methodology applicable across manufacturing, software development, healthcare operations, and professional services.
At its core, the Kanban Method operates on four foundational principles that distinguish it from disruptive organisational change models. First, it advocates starting with existing processes rather than wholesale replacement, minimising resistance and reducing implementation costs. Second, it champions incremental, evolutionary change over revolutionary overhauls. Third, it respects current roles, responsibilities, and organisational structures. Fourth, it encourages leadership at all organisational levels, empowering team members to identify and implement improvements.
For healthcare consultancies managing complex client workflows, appointment scheduling, documentation requirements, and multi-stakeholder coordination, these principles offer particular value. The methodology does not demand organisational restructuring or abandonment of established protocols—instead, it provides a framework for visualising and optimising what already exists.
Research demonstrates compelling outcomes: 87% of organisations implementing Kanban report it as more effective than alternative methods, whilst 86% plan to expand their Kanban initiatives within twelve months. Healthcare operations specifically benefit from Kanban’s ability to manage patient flow, coordinate cross-functional teams, and reduce lead times—with documented cases showing lead time reductions from twelve weeks to two weeks, representing an 83% improvement.
How Does Visual Workflow Management Transform Operational Efficiency?
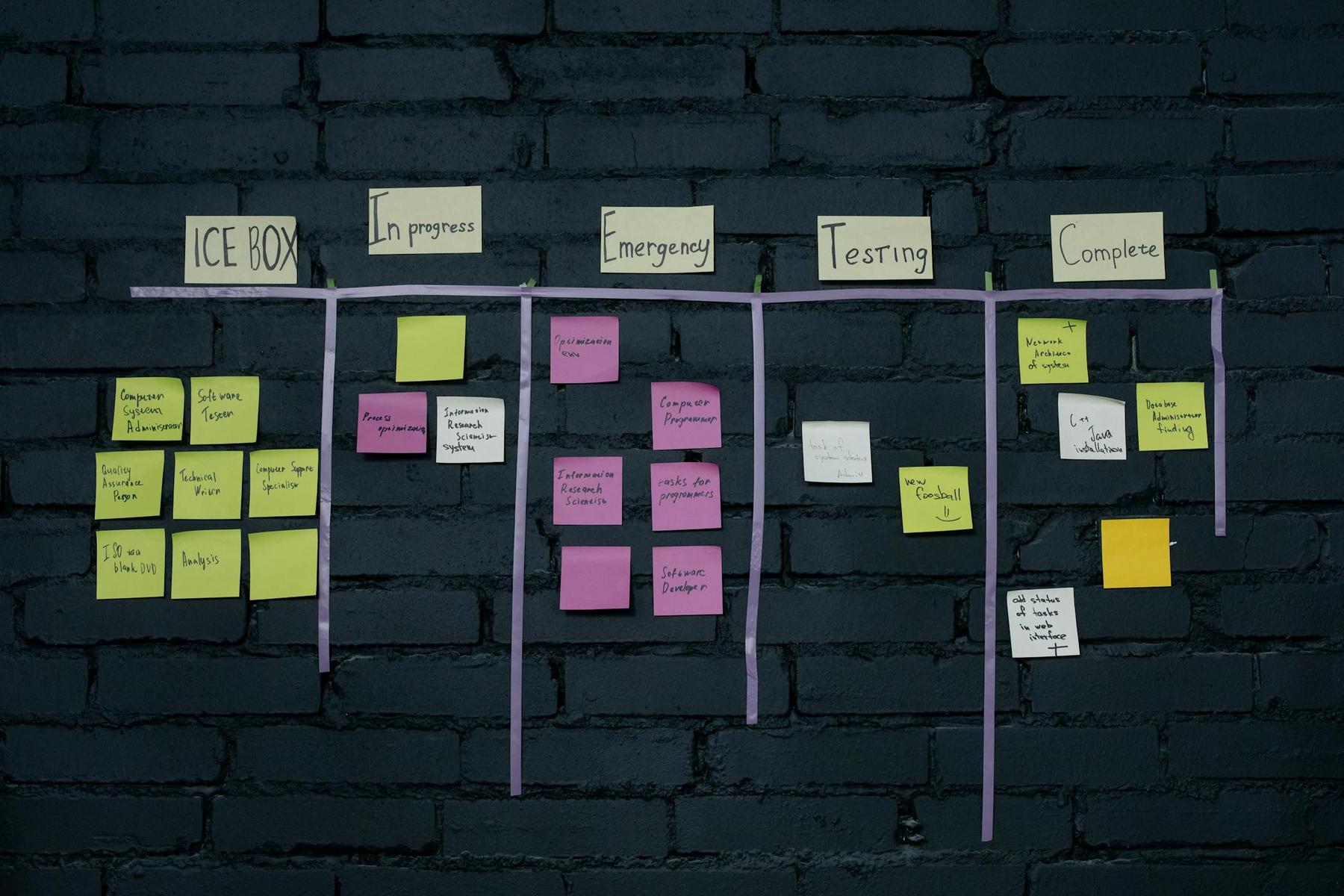
Visual workflow management through Kanban boards transforms abstract work into tangible, trackable items that all team members can observe and understand. A Kanban board comprises columns representing workflow stages (typically beginning with “To Do,” “In Progress,” and “Done”), cards representing individual tasks, and work-in-progress (WIP) limits controlling how many items can occupy each column simultaneously.
This visualisation creates what researchers term a “single source of truth”—eliminating the confusion that arises when work status exists across disconnected spreadsheets, email threads, and individual recollections. For healthcare consultancies coordinating multiple client engagements, regulatory compliance activities, and service delivery tasks, this consolidated visibility proves invaluable.
The mechanics of WIP limits deserve particular attention. By capping the number of tasks allowed in each workflow stage, organisations prevent the productivity-destroying phenomenon of excessive multitasking. Research indicates that context switching between tasks reduces productivity by 5-30 minutes per switch. When team members focus on completing existing work before starting new tasks, cycle times decrease and quality improves.
Consider the operational reality for a consultancy managing client onboarding, ongoing service coordination, and administrative requirements. Without WIP limits, team members might simultaneously juggle fifteen different client matters at various stages of completion. With appropriate WIP limits—often starting conservatively at one task per team member—the workflow becomes sustainable, predictable, and significantly faster.
Empirical evidence supports these outcomes. Organisations implementing Kanban have documented:
- 50% improvement in on-time project delivery
- Up to 30% enhancement in team efficiency through visual management
- 70-90% reduction in production lead times
- 22.17% increase in output (documented in manufacturing applications)
- Up to 80% fewer defects
These metrics translate directly to healthcare consultancy operations: faster client response times, reduced administrative delays, improved service consistency, and enhanced team capacity to manage complex workflows.
What Are the Six Core Practices That Drive Kanban Success?
The Kanban Method operates through six essential practices that work synergistically to optimise workflow:
Visualise the Workflow
Making invisible work visible represents the foundational practice. Healthcare consultancies managing client assessments, documentation workflows, appointment coordination, and stakeholder communications benefit from boards that display every active task. Physical boards using whiteboards and sticky notes suit co-located teams, whilst digital platforms enable distributed teams to maintain real-time visibility.
Limit Work in Progress
WIP limits enforce pull-based workflow where new work enters only when capacity exists. This prevents team overburden and creates natural problem visibility—when work cannot progress, bottlenecks become immediately apparent. Research demonstrates that WIP limits can increase productivity by up to 40% whilst reducing burnout and improving focus.
Manage Flow
Flow management focuses on minimising lead times and maintaining a steady, sustainable pace. Key metrics include cycle time, lead time, and throughput. Cumulative flow diagrams visualise these metrics, revealing bottlenecks and areas for acceleration.
Make Process Policies Explicit
Clear, visible rules governing workflow management reduce confusion and ensure consistency. These policies include definitions of “done” for each stage, prioritisation criteria, acceptance requirements, and conditions for moving tasks between columns. For regulated healthcare environments, explicit policies support compliance whilst facilitating team coordination.
Implement Feedback Loops
Regular feedback mechanisms—daily stand-up meetings, weekly reviews, and retrospectives—ensure continuous process refinement. These sessions gather insights from those performing the work, identify improvement opportunities early, and surface blockers before they compound into major delays.
Improve Collaboratively, Evolve Experimentally
Data-driven, hypothesis-based improvements characterise mature Kanban implementations. Teams identify problems through metrics, propose small experimental changes, test modifications using “safe-to-fail” approaches, measure results, and either adopt or roll back changes based on outcomes. This creates a culture of continuous improvement without disruptive overhauls.
How Do Healthcare Organisations Implement Kanban Effectively?
Successful Kanban implementation follows a structured yet flexible pathway adapted to organisational context. The following table outlines the five-phase implementation framework with key activities and success indicators:
| Implementation Phase | Core Activities | Success Indicators | Typical Duration |
|---|---|---|---|
| Assessment & Planning | Identify processes needing improvement; document current workflows; identify bottlenecks; define desired outcomes; secure leadership support | Clear baseline metrics established; stakeholder buy-in achieved; pain points documented | 2-4 weeks |
| Design | Map workflow as column structure; establish WIP limits; create process policies; design board format; define “done” criteria | Board structure reflects actual workflow; WIP limits set conservatively; policies documented and visible | 1-2 weeks |
| Team Preparation | Assemble cross-functional team; provide Kanban training; address concerns; establish roles; schedule feedback loops | Team understands principles; daily standup schedule confirmed; resistance addressed | 1-2 weeks |
| Pilot & Launch | Deploy Kanban system; conduct daily standups; monitor metrics closely; gather team feedback; maintain board discipline | Board updated daily; WIP limits enforced; baseline metrics tracked; team engagement evident | 4-8 weeks |
| Optimise & Scale | Review metrics; implement incremental improvements; adjust WIP limits; expand to additional teams; document learnings | Measurable improvements in cycle time and throughput; additional teams requesting adoption; continuous improvements implemented | Ongoing |
Critical success factors include starting with simple three-column boards, respecting existing organisational structures, maintaining high board visibility, strictly enforcing WIP limits, conducting regular team communication, measuring everything, and maintaining patience with evolutionary change. Common challenges include resistance to change, overcomplicated boards, inconsistent updates, and insufficient discipline with WIP limits, all of which can be overcome with clear policies and dedicated training.
Why Do Leading Organisations Choose Kanban Over Alternative Methodologies?
Healthcare consultancies evaluating workflow management approaches often compare Kanban against Scrum, Waterfall, and broader Lean implementations. Kanban operates as a continuous flow system without fixed time-boxes, enabling flexible prioritisation and timeline adaptation. Unlike Scrum’s rigid sprint structure, Kanban allows task addition or removal at any time, which is particularly valuable for managing unpredictable client needs and regulatory requirements.
Where Scrum measures velocity within fixed sprints, Kanban tracks cycle time, lead time, and throughput continuously. Scrumban—a hybrid approach combining Scrum’s structured ceremonies with Kanban’s visual workflow management—has emerged as a popular option. Compared to Waterfall’s sequential approach, Kanban’s iterative and adaptive methodology is better suited for environments requiring responsiveness and continuous improvement.
What Measurable Outcomes Can Healthcare Organisations Expect?
Evidence supporting Kanban in healthcare and professional services shows significant operational improvements. Efficiency metrics include a 50% improvement in on-time delivery, up to a 30% enhancement in team efficiency, and a 70-90% reduction in lead times. Quality improvements, such as up to an 80% reduction in defects, also contribute to better service outcomes. Additionally, teams benefit from enhanced morale, increased engagement, and reduced stress due to sustainable workload management.
The 2022 State of Kanban Report highlights improved visibility, faster delivery, and enhanced predictability as key drivers for Kanban adoption. For healthcare consultancies, these outcomes translate to faster client response times, reduced administrative delays, and better overall service quality.
Refining Healthcare Operations Through Visual Management Excellence
The Kanban Method offers healthcare consultancies a proven framework for transforming operational chaos into orchestrated flow. By making work visible, limiting work-in-progress, managing flow metrics, establishing explicit policies, implementing feedback loops, and pursuing collaborative improvement, organisations can adapt to changing demands while maintaining high service quality.
For healthcare consultancies committed to operational excellence, the question shifts from whether to adopt visual workflow management to how quickly implementation can proceed.
How long does Kanban implementation typically take before organisations see measurable results?
Most organisations observe initial improvements within 4-8 weeks of launching their pilot Kanban system, with measurable enhancements in cycle time and team engagement. Full optimisation is an ongoing journey, often spanning 3-4 months from assessment to optimised operation, though simpler workflows may show faster results.
Can Kanban work effectively for small healthcare consultancies with limited team sizes?
Yes, Kanban scales exceptionally well to small organisations. Smaller teams can implement an effective system using a simple board with three columns and conservative WIP limits (typically one task per person), which helps prevent overcommitment and enhances transparency.
What distinguishes successful Kanban implementations from those that fail to deliver value?
Successful implementations maintain strict discipline with WIP limits, invest in proper training, establish clear and visible process policies, and conduct regular daily standups focused on workflow. Failures often stem from overcomplicated board designs, inconsistent updates, and resistance to the evolutionary change principle.
How does Kanban accommodate urgent requests and changing priorities common in healthcare consultancy work?
Kanban’s continuous flow model allows teams to visualise the impact of urgent requests and adjust priorities in real time. Many organisations implement expedite or priority swimlanes on their boards, ensuring that urgent work is managed without derailing ongoing tasks.
What technology investment is necessary for implementing Kanban in a healthcare consultancy?
Initial implementation of Kanban can be achieved with minimal investment using physical boards and sticky notes. As needs evolve, organisations may adopt digital tools like Trello, Asana, or Jira, which offer advanced features such as WIP limit enforcement, real-time collaboration, and compliance with data security regulations.