Every night, millions of Australians climb into bed expecting sleep to arrive naturally—yet for many, the bedroom has become a battleground rather than a sanctuary. The sheets that should signal rest instead trigger restlessness. The pillow that should cradle dreams becomes a prop for racing thoughts. This paradox lies at the heart of sleep associations: the powerful, often invisible conditioning that determines whether our brain interprets bedtime cues as invitations to sleep or signals for wakefulness. With nearly 60% of Australian adults regularly experiencing sleep symptoms and only 1% accessing evidence-based treatment, understanding the mechanisms of conditioned sleep cues has never been more critical for public health.
What Are Sleep Associations and How Do They Form?
Sleep associations represent the environmental or behavioural cues that the brain links with the act of falling asleep through a process called classical conditioning. This psychological mechanism, first demonstrated through Pavlov’s experiments, operates continuously throughout our lives, shaping how we respond to bedtime routines, bedroom environments, and pre-sleep behaviours.
The formation of sleep associations follows specific neurobiological principles. When a neutral stimulus—such as dimming lights, a particular room temperature, or a consistent bedtime routine—repeatedly precedes the onset of sleep, the brain begins to form predictive associations. Over time, these previously neutral cues become conditioned stimuli that trigger physiological and psychological responses associated with sleep onset. This conditioning can be both conscious and unconscious, developing through repetition and reinforcement.
For strong sleep associations to develop, three critical conditions must be met consistently. First, sleep cues must frequently be followed by sleepiness. Second, these cues must rarely occur without subsequent sleepiness. Third, the cues must appear immediately before the onset of sleepiness. When these conditions align, the brain establishes robust neural pathways linking specific environmental signals with sleep states.
The complexity of sleep associations stems from the gradual nature of sleep onset itself. Unlike discrete events, falling asleep involves multiple components occurring along a continuum: physical comfort, feelings of security, progressive drowsiness influenced by both circadian rhythms and accumulated sleep pressure. Each element can become part of the conditioned response, creating intricate networks of associations that either facilitate or inhibit sleep.
The Neurobiological Foundation
The neuroscience underlying sleep associations involves multiple brain regions and neurochemical systems. When positive sleep associations activate, they stimulate the release of neurotransmitters including serotonin and gamma-aminobutyric acid (GABA), which promote relaxation and facilitate the transition to sleep. Conversely, negative associations or stimulus dyscontrol can trigger stress hormone release, particularly cortisol, creating physiological arousal that directly opposes sleep onset.
The suprachiasmatic nucleus (SCN) in the hypothalamus serves as the master circadian pacemaker, orchestrating 24-hour biological rhythms that govern sleep-wake cycles. Environmental cues, particularly light exposure, synchronise this internal clock with the external environment. When sleep associations align with circadian timing, they reinforce natural sleep propensity. When misaligned, they create conflict between learned behaviours and biological readiness for sleep.
How Do Positive and Negative Sleep Associations Impact Sleep Quality?
The dichotomy between positive and negative sleep associations fundamentally shapes sleep quality, with profound implications for both immediate rest and long-term health outcomes. Understanding this distinction provides the foundation for interventions that can transform sleep patterns.
Positive sleep associations function as facilitators, creating environmental and psychological conditions that support natural sleep onset. These include calm, repetitive bedtime routines—such as bathing, reading, or listening to soft music in sequence. Consistency proves paramount: using the same sleep environment with controlled temperature and minimal light exposure, employing white noise to mask disruptive sounds, and even utilising consistent verbal cues like specific phrases associated with bedtime. Environmental elements such as particular scents, comfortable bedding, and predictable timing all contribute to building strong positive associations.
In contrast, negative sleep associations—technically termed stimulus dyscontrol—actively interfere with sleep onset and maintenance. The most common manifestation involves using the bed and bedroom for activities beyond sleep and intimacy. Reading, watching television, working on computers, eating, or using smartphones in bed systematically weakens the bed’s association with sleep whilst strengthening its connection to wakefulness and arousal.
The Cascade Effect of Poor Sleep Associations
When the bedroom becomes associated with frustration, anxiety, and arousal rather than relaxation and rest, a self-perpetuating cycle emerges. The bed transforms into a cue for wakefulness, triggering increased alertness precisely when drowsiness is desired. This phenomenon extends beyond external cues to internal ones: racing thoughts, anticipatory anxiety about not sleeping, and physiological arousal themselves become conditioned triggers for further arousal.
This negative conditioning intensifies through what researchers term “sleep effort”—the conscious attempt to force sleep to occur. Each minute spent lying awake, mentally striving to fall asleep, strengthens the bed-wakefulness association. Over time, this pattern can develop into psychophysiologic insomnia, a disorder characterised by learned sleep-preventing associations that persist even when the original trigger has resolved.
The impact extends to daytime functioning. Australian data reveals that 76% of individuals sleeping less than 5.5 hours report frequent daytime impairment, affecting concentration, mood regulation, and physical health. The economic consequences prove substantial, with sleep-related health issues costing the Australian economy an estimated $75.5 billion in 2019-20, reflecting both direct healthcare expenditure and indirect costs from productivity losses and accidents.
What Role Does Classical Conditioning Play in Sleep Behaviour?
Classical conditioning serves as the fundamental mechanism through which sleep associations form, persist, and can be modified. This learning process, operating largely below conscious awareness, explains why sleep difficulties often resist purely logical or willpower-based solutions.
In classical conditioning applied to sleep, a conditioned stimulus (CS)—such as lying in bed—consistently precedes sleep (the unconditioned stimulus, US). Through repeated pairing, the conditioned stimulus begins to elicit a response similar to sleep onset (the conditioned response, CR). However, sleep’s complexity as an unconditioned stimulus introduces unique challenges. The “comfortable, sleepy feeling” emerges gradually rather than instantaneously, comprising multiple components including physical comfort, psychological security, circadian-driven drowsiness, and homeostatic sleep pressure from accumulated wakefulness.
This gradual onset means that sleep associations form through subtle, repeated experiences rather than singular dramatic events. A person who consistently reads in bed before sleep may develop a reading-sleep association. However, if reading sometimes precedes sleep and sometimes precedes hours of wakefulness, the association weakens or becomes confused. Consistency proves essential for strong conditioning.
Operant Conditioning and Sleep Behaviour
Complementing classical conditioning, operant conditioning influences sleep through consequences and reinforcement. When specific behaviours reliably lead to successful sleep onset, those behaviours become reinforced and more likely to recur. Conversely, behaviours that fail to produce sleep—or worse, prolong wakefulness—should theoretically decrease through extinction. However, the intermittent reinforcement inherent in insomnia (occasionally falling asleep despite poor sleep hygiene) can paradoxically strengthen maladaptive behaviours.
Stimulus control therapy, the most effective single behavioural treatment for insomnia, directly targets these conditioning processes. By systematically strengthening the bed and bedroom as cues for sleep whilst weakening their association with arousal and wakefulness, stimulus control therapy reconditions the sleep environment through both classical and operant mechanisms.
How Can Environmental Cues Strengthen Sleep Associations?
Environmental cues, termed zeitgebers (“time givers” in German), represent the external signals that synchronise internal biological rhythms with the external world. Three primary zeitgebers exert particularly powerful influences on sleep associations and circadian entrainment: light exposure, meal timing, and exercise timing.
Light Exposure: The Primary Zeitgeber
Light exposure dominates as the most powerful environmental cue for sleep-wake regulation. The suprachiasmatic nucleus processes light information detected by specialised photoreceptors in the eyes, particularly sensitive to blue-light wavelengths. This information either advances, delays, or maintains circadian timing depending on when exposure occurs.
Morning light exposure advances the circadian rhythm, promoting earlier sleep onset and wake times. Evening light exposure delays the rhythm, shifting sleep timing later. Remarkably, natural sunlight proves significantly more powerful than artificial lighting for circadian entrainment. Research demonstrates that participants exposed to natural light-dark cycles showed approximately two hours earlier melatonin onset compared to those in electrical lighting environments, underscoring the profound disconnect between modern indoor lifestyles and evolutionarily adapted circadian systems.
The implications for sleep associations are substantial. Consistent morning light exposure strengthens the association between dawn and awakening, whilst dimming lights in evening hours reinforces the brain’s interpretation of darkness as a sleep signal. Blue light from electronic devices suppresses melatonin production, the primary hormone regulating sleep-wake cycles, directly interfering with sleep onset associations.
Meal Timing and Exercise as Secondary Zeitgebers
Meal timing represents the second most powerful environmental cue for circadian regulation, particularly influencing peripheral organs’ circadian rhythms. When caloric intake begins, organs shift from rest and rejuvenation processes to digestive functions. Late evening eating truncates organ rest periods, potentially disrupting sleep quality and metabolic health. Consistent meal timing reinforces circadian regularity, strengthening associated sleep-wake patterns.
Exercise timing occupies the third position in zeitgeber hierarchy. Physical activity influences circadian phase and melatonin production timing. Morning or afternoon exercise generally supports optimal circadian alignment, whilst vigorous evening exercise can delay sleep onset by increasing core body temperature and arousal when the body should be cooling for sleep.
Why Are Sleep Associations Critical for Australian Sleep Health?
The Australian sleep health landscape reveals a crisis of both prevalence and treatment access, making understanding and addressing sleep associations particularly urgent. Current data paints a concerning picture of widespread sleep disruption with minimal utilisation of evidence-based interventions.
| Sleep Health Metric | Prevalence | Notes |
|---|---|---|
| Adults with regular sleep symptoms (3+ times/week) | 59.4% | Approximately 14.8 million adults affected |
| Clinical insomnia diagnosis criteria | 14.8% | More common in females (25.2%) than males (21.1%) |
| Chronic insomnia disorder (ICSD-3 criteria) | 23.2% | Higher in those under 55 years (26.4%) |
| Difficulty falling asleep | 33% | More frequent in younger adults (32% of 18-24 year-olds) |
| Difficulty staying asleep | 33% | More common in older adults (47% of 65+ years) |
| Sleep less than 5.5 hours | 12% | 76% report frequent daytime impairment |
| Discussed sleep with GP | 37% | Among those with chronic insomnia symptoms |
| Received CBT-I | <1% | Despite being recommended first-line treatment |
These statistics reveal several critical patterns. First, sleep problems affect the majority of Australian adults, suggesting systemic issues with sleep associations in modern society. Second, significant demographic variations exist, with younger females particularly affected by chronic insomnia (26.4% prevalence). Third, and perhaps most troubling, only 37% of people with chronic insomnia symptoms have discussed sleep with their general practitioner, and fewer than 1% have accessed cognitive behavioural therapy for insomnia (CBT-I), despite its designation as first-line treatment by the American College of Physicians and supported by Australian guidelines.
The Treatment Gap and Its Consequences
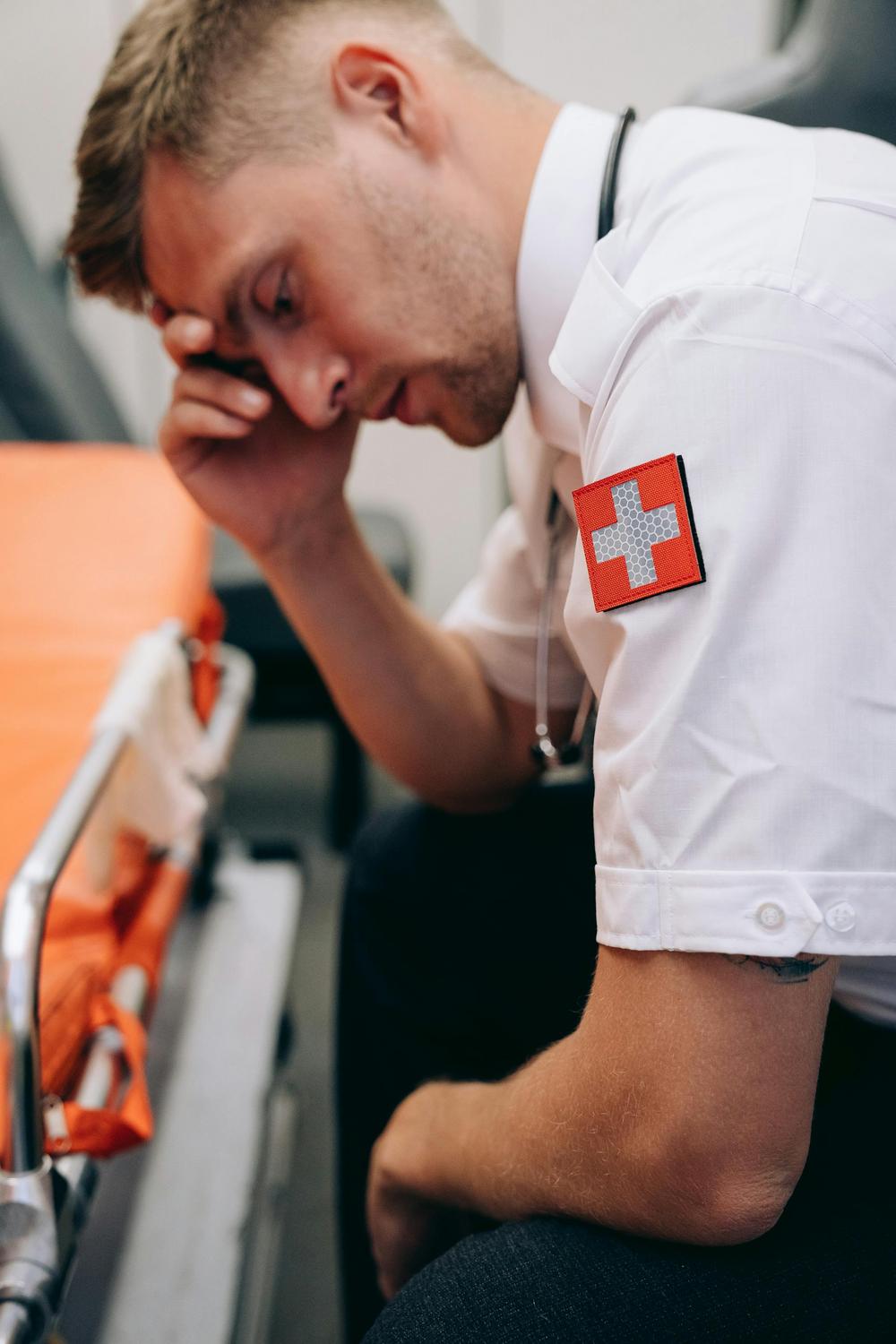
The disparity between sleep problem prevalence and treatment access represents a critical failure in healthcare delivery. Multiple factors contribute to this gap: time pressures on general practitioners, low prioritisation of sleep complaints, limited provider knowledge about sleep interventions, and inadequate access to psychologists trained in CBT-I delivery.
This treatment gap carries profound consequences. Sleep problems disproportionately affect vulnerable populations including Aboriginal and Torres Strait Islander communities, shift workers, and those in rural and remote areas. The economic burden—$75.5 billion annually—reflects costs spanning direct healthcare expenditure, productivity losses, workplace accidents, and motor vehicle crashes. Alarmingly, 29% of Australians drive whilst drowsy monthly, and 20% report having nodded off whilst driving, directly linking poor sleep associations to road safety.
The demographic patterns merit particular attention. Females consistently report higher rates of sleep problems: 31% of females versus 21% of males “often or always” worry about obtaining good sleep, whilst 35% of females versus 25% of males feel overwhelmed by thoughts when attempting sleep. These differences suggest that gender-specific factors—potentially including hormonal variations, caregiving responsibilities, and psychosocial stressors—interact with sleep associations to create differential vulnerability.
What Evidence-Based Approaches Reshape Sleep Associations?
Fortunately, robust evidence demonstrates that sleep associations, even long-established ones, can be systematically modified through targeted interventions. These approaches leverage the same conditioning principles that formed problematic associations to establish healthier patterns.
Stimulus Control Therapy: The Foundation
Stimulus control therapy (SCT), developed by Bootzin in 1972, remains the most effective single behavioural treatment for insomnia. The approach systematically strengthens the bed and bedroom as discriminative stimuli for sleep whilst weakening their association with arousal and wakefulness. Based on operant learning theory, SCT treats falling asleep as an instrumental act subject to reinforcement through consequences.
The core instructions exemplify elegant simplicity: go to bed only when genuinely sleepy rather than by clock time; use the bed and bedroom exclusively for sleep and intimacy; if unable to fall asleep within 15-20 minutes, leave the bed and engage in relaxing activity elsewhere; return to bed only when sleepy; maintain consistent wake time every morning regardless of sleep quality; avoid daytime napping. These guidelines deliberately create conditions where bed consistently predicts sleep onset, reconditioning the association through repeated successful pairings.
The effectiveness of stimulus control therapy has been demonstrated across numerous studies, with the American Academy of Sleep Medicine identifying it as effective and recommended therapy for chronic insomnia. Effect sizes equal those of sleep restriction therapy, and SCT proves particularly effective for sleep onset problems occurring at the beginning or middle of the night. Beyond symptom improvement, stimulus control therapy strengthens patients’ perceived control over insomnia, reducing the distress that perpetuates sleep difficulties.
Sleep Restriction Therapy: Leveraging Sleep Homeostasis
Sleep restriction therapy (SRT) approaches sleep associations through a complementary mechanism: manipulating homeostatic sleep pressure to consolidate sleep and strengthen its association with bedtime. The intervention systematically limits time in bed to match actual sleep time, increasing sleep drive through controlled sleep deprivation. This approach exploits the fundamental principle that longer wakefulness increases sleep likelihood.
The protocol begins by calculating average total sleep time through sleep diaries, then restricting time in bed to match that duration (never below five hours to prevent excessive daytime drowsiness). As sleep efficiency improves, the sleep window gradually expands by 15-20 minutes weekly if sleep efficiency exceeds 90%. This controlled process helps re-entrain dysregulated circadian rhythms whilst rebuilding the association between lying down and rapidly falling asleep.
Cognitive Behavioural Therapy for Insomnia: Comprehensive Reconditioning
Cognitive behavioural therapy for insomnia (CBT-I) represents the gold standard intervention, combining multiple evidence-based components into a comprehensive treatment package. The multimodal approach addresses sleep associations through several simultaneous mechanisms: stimulus control instructions target bed-sleep conditioning, sleep restriction regulates sleep homeostasis, sleep hygiene education modifies behavioural factors, Cognitive restructuring addresses dysfunctional beliefs about sleep, relaxation training reduces arousal, and psychoeducation provides framework understanding.
The evidence supporting CBT-I proves remarkably robust. More than 50 randomised controlled clinical trials demonstrate reliable, robust improvements, with 70-80% of patients with primary insomnia experiencing significant benefits. These include reduced time to fall asleep, increased total sleep time, and decreased nocturnal awakenings. Crucially, benefits typically persist after treatment concludes, with improvements sustained long-term as the reconditioned sleep associations remain stable.
CBT-I effectiveness extends across diverse populations and contexts. The intervention proves effective for insomnia secondary to chronic pain and cancer, across all age groups including elderly populations, and demonstrates substantial effectiveness with particular strength in long-term outcomes as the reconditioned sleep associations provide lasting benefits. This combination of efficacy, durability, and absence of adverse effects explains its designation as first-line treatment by major medical organisations.
The Cognitive Component: Addressing Mental Associations
The cognitive therapy elements of CBT-I specifically target mental and emotional associations with sleep. Many individuals with chronic insomnia develop dysfunctional thoughts about sleep—unrealistic expectations about required sleep duration, catastrophic interpretations of poor sleep consequences, anxiety about past insomnia experiences, and excessive worry about daytime fatigue. These cognitive patterns create emotional arousal that becomes conditioned to bedtime, forming internal cues that trigger wakefulness.
Cognitive restructuring systematically identifies and challenges these thought patterns, replacing them with more realistic, less anxiety-provoking interpretations. This process directly weakens the association between bedtime and anxiety whilst building new associations between bedtime and calm acceptance.
Relaxation Techniques: Reducing Somatic Arousal
Complementing stimulus control and cognitive approaches, relaxation techniques target the somatic hyperarousal characteristic of insomnia. Progressive muscle relaxation (PMR), which has the strongest research support, involves systematically tensing and relaxing muscle groups, conditioning the body to recognise and achieve relaxed states. Breathing exercises, autogenic training, imagery techniques, meditation, and biofeedback each offer pathways to reduce physiological arousal that interferes with sleep onset.
These techniques prove particularly effective for individuals characterising their insomnia as an “inability to relax” and those with prominent somatic complaints. However, some patients may experience paradoxical responses, particularly those with panic disorder history or performance anxiety. Careful assessment and individualised application optimise outcomes.
Building Sustainable Sleep Associations for Long-Term Health
Reshaping sleep associations requires recognising that breaking negative patterns alone proves insufficient—the focus must centre on building new, positive associations through consistent practice and environmental management. Unlike cognitive skills learned once and retained, conditioned responses require ongoing reinforcement to maintain strength.
The principle of association formation dictates that new cues must immediately and consistently precede desired responses. For sleep associations, this means establishing unwavering consistency in pre-sleep routines, sleep timing, and environmental conditions. The bedroom environment itself requires careful curation: darkness, appropriate temperature, minimal noise, comfortable bedding, and absence of work-related materials or electronic devices all contribute to strengthening sleep-specific associations.
Circadian rhythm management through strategic environmental cue manipulation amplifies these effects. Morning light exposure—ideally natural sunlight—advances circadian timing and reinforces morning alertness associations. Evening light reduction, particularly limiting blue light from screens in the two hours before bed, strengthens darkness-sleep associations. Consistent meal timing, with the last substantial meal occurring several hours before bedtime, supports both circadian regularity and digestive comfort during sleep.
Physical activity timing requires consideration of individual circadian preference and response. For most individuals, morning or early afternoon exercise supports better sleep without interfering with evening wind-down. However, some individuals tolerate later exercise well. The key lies in consistency—exercising at similar times daily strengthens circadian entrainment whilst building predictable daily rhythm associations.
The psychological dimension of sustainable sleep associations encompasses stress management and time management strategies that prevent bedtime from becoming associated with worry and rumination. Establishing a “worry time” earlier in the evening—a designated period for addressing concerns and planning—helps quarantine anxiety from bedtime. Similarly, maintaining engaging hobbies and recreational pursuits ensures that wakefulness is associated with fulfilling activities, making the transition to sleep a natural conclusion rather than an enforced cessation of stimulation.
The Role of Professional Guidance
Whilst general sleep hygiene principles prove accessible to all, individuals with persistent sleep difficulties benefit substantially from professional guidance. The complex interactions between conditioning, circadian rhythms, cognitive patterns, and medical factors often require expert assessment to disentangle. Moreover, the low access rates to evidence-based treatment in Australia—fewer than 1% receiving CBT-I despite its first-line status—suggest that expanding treatment availability represents a critical public health priority.
Healthcare providers trained in sleep medicine can assess for underlying sleep disorders, optimise intervention timing and intensity, monitor progress through objective measures, and adjust approaches based on individual response. For individuals with comorbid medical or psychological conditions, integrated treatment addressing multiple factors simultaneously optimises outcomes.
Emerging Research and Future Directions
Recent research has revealed surprising capabilities for learning during sleep itself, opening new frontiers in understanding sleep associations. Studies demonstrate that novel associations can form during sleep through implicit learning processes—learning that occurs without conscious awareness and sometimes proves more effective than explicit waking learning. Remarkably, olfactory conditioning during sleep can modify subsequent waking behaviour, with effects persisting for days and varying by sleep stage. These findings suggest that sleep states themselves may offer unique windows for association formation and modification.
The integration of technology into sleep monitoring and intervention continues evolving. Wearable devices tracking sleep patterns, environmental sensors monitoring bedroom conditions, and smartphone applications delivering CBT-I components all promise to expand treatment access. However, these technologies must be implemented carefully to avoid creating new negative associations—obsessive sleep tracking can itself generate anxiety that interferes with sleep.
How long does it take to establish new sleep associations?
Establishing new sleep associations through consistent practice typically requires several weeks to several months, depending on the strength of existing associations and the consistency of new patterns. Research on stimulus control therapy and CBT-I demonstrates measurable improvements often beginning within two to four weeks, with continued strengthening over subsequent months. Individual variation is substantial, so patience and persistence are key.
Can positive sleep associations formed in childhood affect adult sleep quality?
Yes, sleep associations established during childhood can influence adult sleep patterns. Children who develop positive sleep associations through consistent routines and environments often carry these habits into adulthood. Conversely, negative associations from childhood can predispose individuals to adult insomnia. However, these patterns can be modified later in life through targeted interventions.
Why do sleep associations sometimes stop working suddenly?
Sleep associations can appear to fail when other factors, such as significant life stress, circadian misalignment from schedule changes, medical issues, or environmental alterations, override their effects. While the underlying associations may remain, their effectiveness can be diminished if contradictory cues are introduced or if external factors trigger arousal at bedtime.
Do sleep associations work differently for shift workers?
Shift workers face unique challenges because their sleep timing often conflicts with natural circadian rhythms. However, the principles of conditioning still apply. By creating consistent pre-sleep routines, controlling environmental cues (like light and noise), and strategically timing exposure to zeitgebers, shift workers can modify their sleep associations to better align with their atypical schedules.
Are sleep associations affected by sleeping in different locations?
Sleeping in unfamiliar locations can disrupt established sleep associations due to the “first night effect,” where heightened vigilance in a new environment affects sleep quality. Nevertheless, maintaining consistent pre-sleep routines and bringing familiar items (such as a favorite pillow or blanket) can help mitigate these disruptions and preserve portable sleep associations.