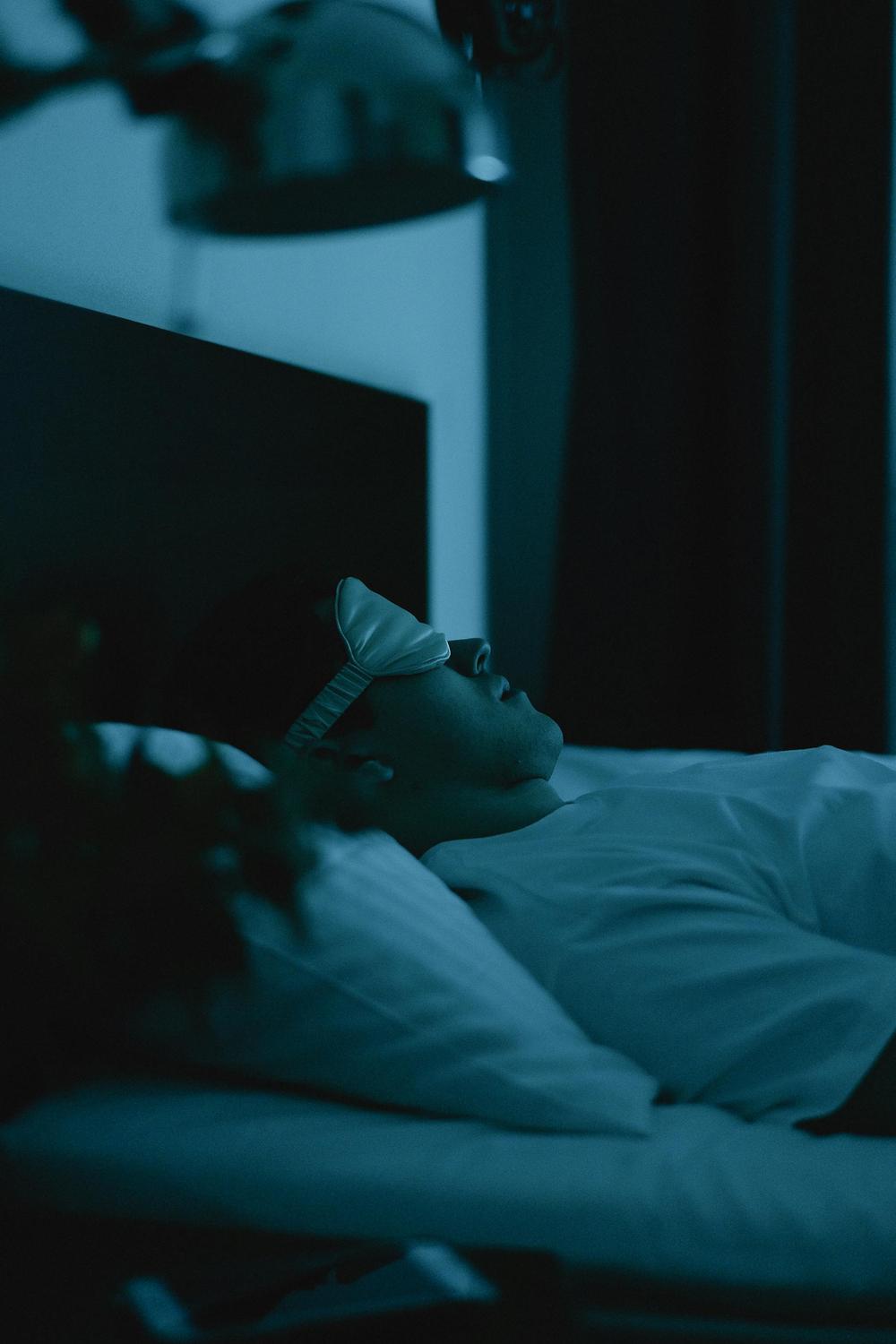
The image is unsettling yet strangely familiar: a family member wandering through the house in the dead of night, eyes open but unseeing, moving with purpose yet entirely unaware. By morning, they’ll have no memory of their nocturnal journey. This phenomenon—somnambulism, more commonly known as sleepwalking—affects millions worldwide, yet remains one of sleep medicine’s most fascinating and poorly understood conditions.
For families confronting this reality, the questions multiply faster than the answers. Why does it happen? Is it dangerous? Will it ever stop? Beyond the immediate concerns about safety and sleep disruption lies a deeper mystery: what exactly is happening in the brain when someone walks, talks, or even performs complex tasks whilst fundamentally asleep?
Somnambulism represents far more than an inconvenient quirk of sleep. It stands at the intersection of neuroscience, genetics, and environmental factors, offering profound insights into how our brains transition between consciousness and unconsciousness. Understanding this condition requires examining not just what happens during episodes, but why certain individuals are susceptible, how the condition manifests across different life stages, and what modern science reveals about this ancient phenomenon.
What Is Somnambulism and How Common Is It?
Somnambulism, derived from the Latin words meaning “sleep” and “walking,” represents a specific type of parasomnia—abnormal behaviours occurring during sleep that fall on the border between sleep and wakefulness. Clinically classified as a disorder of arousal from non-rapid eye movement (NREM) sleep, somnambulism specifically emerges during N3 sleep, the deepest stage of the sleep cycle also known as slow-wave sleep.
The defining characteristic that distinguishes true somnambulism from other sleep disorders is the occurrence of complex motor behaviours or ambulation during partial arousal from deep sleep, combined with complete or near-complete amnesia for the episode. This memory loss is not simply forgetting—it represents a fundamental failure of the brain to encode experiences during the episode, as consciousness remains profoundly altered throughout.
The global prevalence of somnambulism reveals striking patterns across the lifespan. A comprehensive meta-analysis examining 51 studies with over 100,000 participants established that 6.9% of the population experiences sleepwalking at some point during their lifetime. However, current prevalence—episodes occurring within the past 12 months—differs dramatically by age group. Amongst children, 5.0% actively experience sleepwalking, whilst only 1.5% of adults report recent episodes.
The peak prevalence occurs during childhood, specifically between ages 8 and 12 years. Some research indicates rates as high as 17% amongst children and 4% amongst adults in certain populations. This age distribution reflects fundamental changes in brain development and sleep architecture across the lifespan.
Within the Australian context, approximately 22% of adults have doctor-diagnosed sleep disorders, with parasomnias like somnambulism representing a significant subset of these cases. Australian research has contributed substantially to understanding the epidemiology of sleepwalking, particularly regarding associations with children’s sleep behaviours and bedtime routines.
The chronicity of somnambulism presents another critical dimension. Studies demonstrate that over 80% of individuals who sleepwalk experience episodes lasting more than five years, with 22.8% of clinical sleepwalkers having nightly episodes and 43.5% experiencing weekly occurrences. This persistent nature underscores the importance of proper assessment and management strategies.
Why Does Sleepwalking Occur? Understanding the Causes and Risk Factors
Despite decades of research, the exact mechanisms underlying somnambulism remain incompletely understood. However, one causal factor stands definitively established: genetic predisposition represents the primary, most well-documented risk factor for somnambulism.
The Genetic Foundation
The hereditary nature of sleepwalking cannot be overstated. If one parent has a history of sleepwalking, their child faces a 47% probability of developing the condition. When both parents have experienced somnambulism, this risk escalates to 61%. In stark contrast, only 22% of children with no family history will sleepwalk at least once—a nearly threefold increase in risk when genetic factors are present.
Twin studies provide compelling evidence for genetic influence. Monozygotic (identical) twins demonstrate concordance rates of approximately 55% for childhood sleepwalking, compared to 35% in dizygotic (fraternal) twins. For adult sleepwalking, identical twins show 5.3 times greater concordance than fraternal twins.
Recent genetic research has identified specific loci associated with increased sleepwalking risk. The HLA-DQB1*05 gene mutation shows association with higher sleepwalking prevalence in white populations. Genome-wide association studies have pinpointed chromosome 20q12-q13.12 as the first genetic locus definitively linked to somnambulism, with additional risk loci identified on chromosome 18 in African American populations.
Sleep Deprivation: A Powerful Trigger
Beyond genetic predisposition, sleep deprivation stands as the most significant modifiable risk factor. Lack of adequate sleep increases both the likelihood and severity of sleepwalking episodes. Remaining awake for more than 24 hours significantly elevates sleepwalking risk, as sleep deprivation promotes increased slow-wave sleep during recovery periods—precisely the sleep stage during which somnambulism occurs.
Stress and Emotional Factors
Psychological stress—whether work-related, academic, or personal—demonstrates strong association with sleepwalking episodes. Anxiety disorders, depression (associated with 3.5 times higher likelihood), obsessive-compulsive disorder, and post-traumatic stress disorder all correlate with elevated somnambulism rates. Childhood trauma particularly links to increased sleepwalking risk, highlighting the complex interplay between emotional regulation and sleep architecture.
Sleep Schedule Disruptions and Environmental Factors
Irregular sleep schedules, shift work, travelling and sleeping in unfamiliar environments, and disrupted circadian rhythms all contribute to sleepwalking risk. Environmental triggers include loud noises exceeding 100 decibels, physical touch, full bladder, and noisy sleep environments. These factors can trigger episodes in genetically predisposed individuals by creating arousals during slow-wave sleep.
Comorbid Sleep Disorders
Obstructive sleep apnoea (OSA) represents a particularly significant trigger, as sleep interruptions and arousals can precipitate sleepwalking episodes. Restless legs syndrome, sleep-disordered breathing, and periodic limb movement disorder all demonstrate association with increased parasomnia frequency. Notably, treatment of these underlying conditions often resolves associated sleepwalking.
Medical and Neurological Conditions
Various medical conditions associate with increased somnambulism risk. Neurological conditions including Parkinson’s disease, stroke, and traumatic brain injury can trigger sleepwalking in previously unaffected individuals. Thyroid dysfunction, particularly hyperthyroidism, gastro-oesophageal reflux disease, and fever (especially in children) all correlate with elevated sleepwalking rates.
Migraine sufferers demonstrate 4-6 times increased likelihood of sleepwalking, whilst individuals with Tourette syndrome show 4-9 times elevated risk—both conditions potentially sharing underlying serotonin-related mechanisms.
Hormonal Influences
Hormonal fluctuations affect sleepwalking patterns, particularly in women. The premenstrual period shows higher likelihood of episodes, whilst pregnancy may actually decrease sleepwalking occurrence despite significant hormonal changes.
| Risk Factor Category | Specific Examples | Relative Risk/Impact |
|---|---|---|
| Genetic | One parent affected | 47% risk to child |
| Both parents affected | 61% risk to child | |
| No family history | 22% baseline risk | |
| Sleep-Related | Sleep deprivation | Significant increase |
| Obstructive sleep apnoea | Strong trigger; treatment often resolves sleepwalking | |
| Irregular sleep schedule | Moderate increase | |
| Psychological | Depression | 3.5x higher likelihood |
| Anxiety disorders | Elevated risk | |
| PTSD/trauma | Increased association | |
| Medical | Migraine headaches | 4-6x more likely |
| Tourette syndrome | 4-9x more likely | |
| Fever (in children) | Increased likelihood | |
| Environmental | Loud noises (>100 dB) | Can trigger episodes |
| Unfamiliar sleeping location | Moderate trigger | |
| Full bladder | Minor trigger |
What Happens During a Sleepwalking Episode? Understanding the Manifestations
The phenomenology of somnambulism varies dramatically in complexity and duration, ranging from simple sitting up in bed to elaborate behaviours indistinguishable from waking activities.
The Brain’s Paradoxical State
Contrary to popular misconception, sleepwalking does not occur during REM (rapid eye movement) sleep when vivid dreams typically manifest. Instead, somnambulism emerges during N3 sleep—the deepest stage of NREM sleep, characterised by delta waves (the lowest frequency, highest amplitude brain waves). During this stage, the arousal threshold reaches its peak, making awakening most difficult.
Advanced neuroimaging using SPECT (single-photon emission computed tomography) reveals the paradoxical brain state underlying sleepwalking: simultaneous activation of sleeping and waking neural circuits. Studies demonstrate decreased cerebral blood flow in frontal and parietal regions, particularly the dorsolateral prefrontal cortex and insula—areas critical for conscious decision-making, judgement, and environmental awareness.
This selective activation and hypoactivation of neural circuits explains the characteristic behaviours: the motor cortex functions sufficiently for complex movements, whilst higher cognitive centres remain largely dormant, resulting in diminished awareness, impaired judgement, and absent memory consolidation.
Physical Manifestations
Episodes typically commence 1-2 hours after sleep onset when slow-wave sleep predominates. The sleepwalker’s eyes often remain open, displaying a characteristic glassy or blank stare with dilated pupils and no response to environmental stimuli within their visual field. Movements may appear clumsy or gangly, though some individuals execute surprisingly coordinated actions.
Behaviours range from simple (sitting up, walking around) to remarkably complex (getting dressed, preparing food, rearranging furniture, operating vehicles). Speech may occur but typically remains incoherent or nonsensical. Physical sensation diminishes significantly—sleepwalkers may sustain injuries without awareness until morning.
The duration of episodes varies considerably. Most last several minutes, though they can extend from mere seconds to over 30 minutes. Episodes typically conclude when arousal becomes complete or when the individual returns to uninterrupted sleep.
The Hallmark Feature: Amnesia
Complete or near-complete memory loss for episodes represents the diagnostic hallmark of somnambulism. This amnesia differs fundamentally from simple forgetting—the brain fails to encode experiences during episodes due to the altered state of consciousness. Individuals typically learn about their sleepwalking from family members or discover indirect evidence (misplaced objects, unexplained injuries) upon waking.
Difficulty Arousing and Confusion
Awakening a sleepwalker proves remarkably difficult due to the depth of N3 sleep. If successfully roused, the individual experiences pronounced confusion and disorientation lasting several minutes to over an hour—a phenomenon termed “sleep inertia.” During this period, cognitive testing reveals moderately impaired mental performance.
Rare but Serious Behaviours
Whilst most sleepwalking involves benign activities, documented cases include potentially dangerous behaviours: sleep-related eating (consuming unusual food combinations or inedible items), inappropriate urination in unexpected locations, leaving premises through doors or windows, and exceedingly rare instances of aggressive behaviour or sexual activity (sexsomnia) without conscious awareness.
How Is Somnambulism Diagnosed? The Clinical Approach
Diagnosing somnambulism relies primarily on comprehensive clinical assessment rather than sophisticated testing, though specific investigations prove valuable in particular scenarios.
The Foundation: Detailed Clinical History
The most important diagnostic tool remains a thorough history, encompassing age of onset, frequency and timing of episodes, detailed descriptions of behaviours, identified triggers, sleep-wake patterns, family history of parasomnias, and comprehensive medical, psychiatric, and neurological background.
Witness reports from family members or bed partners provide critical diagnostic information, as affected individuals typically possess no direct memory of episodes. Home videos captured on mobile phones or security systems offer invaluable objective documentation, though sleepwalking’s episodic nature makes consistent capture challenging.
Sleep diaries tracking patterns, timing, and potential triggers help establish connections between precipitating factors and episodes, informing both diagnosis and management strategies.
Polysomnography: The Gold Standard with Limitations
Polysomnography (overnight sleep study) represents the gold-standard confirmatory test when sleepwalking occurs during monitoring. This comprehensive assessment records brain activity via electroencephalography (EEG), breathing patterns, muscle activity, and body movements throughout sleep.
However, significant practical limitations exist. Episodes rarely manifest in laboratory settings—the unfamiliar environment, monitoring equipment, and altered routine often suppress behaviours. When episodes do occur in laboratories, they typically appear less complex than home manifestations.
Consequently, polysomnography is not routinely recommended for straightforward cases. Clinical guidelines suggest sleep studies when sleepwalking begins in adulthood, causes significant daytime consequences, involves dangerous behaviours, presents with complex or unusual movements, or when diagnostic uncertainty exists.
Additional Investigations
Electroencephalography may help exclude seizure disorders—an important differential diagnosis—particularly when episodes display stereotyped patterns or occur multiple times nightly. Sleep-deprived EEG sometimes enhances diagnostic sensitivity.
Brain imaging (MRI or CT scanning) becomes relevant for adult-onset cases or when neurological features raise concern about structural abnormalities. Thyroid function testing screens for hyperthyroidism in adult presentations.
Diagnostic Criteria and Classification
The International Classification of Sleep Disorders, Third Edition, Text Revision (ICSD-3-TR) provides formal diagnostic criteria. Key requirements include incomplete arousal from NREM sleep, episodes typically occurring in the first third of the night, complex motor behaviours or ambulation during sleep, diminished environmental awareness, difficulty arousing during episodes, amnesia for events, and absence of significant cognitive impairment upon final awakening.
The condition also appears in ICD-11 (International Classification of Diseases) as a disorder of arousal from NREM sleep, and in DSM-5-TR (Diagnostic and Statistical Manual of Mental Disorders) as a sleep-wake disorder, requiring associated distress or functional impairment for formal diagnosis.
What Are the Risks Associated with Sleepwalking?
Whilst somnambulism typically manifests as a benign condition, potential complications warrant serious consideration, particularly regarding injury risk and quality of life impacts.
Injury Risk and Documented Complications
Falls represent the most common injury mechanism. Sleepwalkers may tumble down stairs, from beds, or from heights, potentially sustaining fractures, head trauma, or other significant injuries. Documented cases include individuals jumping from third-floor windows, resulting in multiple fractures and serious head injuries.
Collisions with objects, doors, and furniture cause trauma ranging from minor bruises to substantial injuries. Walking through glass doors or windows presents particular danger. Rare cases involve self-injury with sharp implements encountered during sleep.
Research examining 620,000 emergency department admissions identified 11 cases directly attributable to sleepwalking trauma, with 36.4% requiring hospital admission for orthopaedic injuries. Broader studies indicate that 7% of sleepwalkers report either witnessing injury or sustaining injury themselves, whilst 17% of individuals in clinical studies experienced at least one episode requiring medical care.
Sleep Disruption and Psychosocial Impact
Beyond physical safety, somnambulism disrupts sleep quality for both affected individuals and household members. The condition associates with higher rates of excessive daytime sleepiness, insomnia symptoms, nightmares (twice as likely as non-sleepwalkers), and reduced sleep satisfaction.
Embarrassment from episodes—particularly those involving inappropriate behaviour or locations—creates significant psychosocial burden. Adults who sleepwalk report higher workplace stress levels and reduced productivity. Children with chronic sleepwalking demonstrate associations with behavioural problems and difficulties with emotional regulation.
Rare but Serious Concerns
Whilst exceedingly uncommon, aggressive behaviour during sleepwalking episodes has been documented, most frequently when individuals are startled or restrained during episodes. Fear represents the most common emotion during events, potentially triggering fight-or-flight responses. Male sleepwalkers more commonly manifest agitated or aggressive behaviours.
The disorientation and confusion upon awakening can occasionally provoke fear or anger responses, though these typically resolve within minutes as full consciousness returns.
How Can Sleepwalking Be Managed? Evidence-Based Approaches
The management of somnambulism requires individualised assessment balancing the frequency and severity of episodes against potential intervention risks and benefits.
When Treatment Becomes Necessary
Most cases of sleepwalking, particularly in children, require no specific intervention. The condition typically proves benign and self-limited. Treatment consideration becomes appropriate when episodes occur more than 1-2 times weekly, cause distress to the individual or family members, lead to dangerous behaviours or injuries, significantly disrupt household sleep, contribute to daytime fatigue or functional impairment, or persist into adulthood after childhood onset.
Safety Measures: The Critical Foundation
Environmental safety modifications represent the cornerstone of management for all cases. Essential precautions include:
- Securing windows and external doors with locks (but never locking individuals in rooms due to fire safety concerns)
- Removing breakable objects, sharp implements, and electrical cords from sleeping areas
- Clearing floors of tripping hazards
- Installing stair gates where appropriate
- Padding areas near beds
- Utilizing motion-sensor lighting
- Implementing door or bed alarms
- Considering first-floor sleeping arrangements when possible
- Removing furniture with sharp corners
- Potentially establishing separate sleeping arrangements if safety concerns exist
Scheduled Waking: The Most Evidence-Based Behavioural Intervention
Anticipated or scheduled waking represents the most rigorously studied and effective non-pharmacological approach. This technique involves waking the individual 15-30 minutes before their typical sleepwalking time, ensuring full wakefulness for several minutes, then allowing return to sleep. Continued nightly for 2-3 weeks, this method interrupts the sleepwalking cycle with minimal adverse effects.
The approach demonstrates effectiveness across age groups and provides a safe, practical first-line intervention for recurrent episodes. Success rates compare favourably to other behavioural approaches whilst avoiding potential complications.
Sleep Hygiene and Lifestyle Modifications
Whilst empirical evidence specifically for sleepwalking treatment remains limited, optimising sleep hygiene provides supportive benefits:
- Maintaining consistent sleep schedules (including weekends)
- Ensuring adequate total sleep duration to prevent sleep deprivation
- Limiting stimulating beverages during evening hours
- Creating comfortable sleep environments (cool, dark, quiet)
- Limiting stimulating activities before bedtime
- Practising relaxation techniques
- Maintaining regular daytime physical activity
Addressing Underlying Conditions
Treating comorbid sleep disorders often dramatically improves or resolves sleepwalking. Obstructive sleep apnoea management through appropriate interventions frequently eliminates associated parasomnias. Similarly, addressing restless legs syndrome, periodic limb movement disorder, or sleep-disordered breathing reduces arousal frequency, thereby decreasing sleepwalking episodes.
When substance effects or environmental factors trigger episodes, modification or elimination often proves curative. Reviewing and potentially adjusting elements that disrupt sleep architecture may resolve somnambulism without additional intervention.
Hypnosis: A Second-Line Behavioural Approach
Clinical hypnosis, whilst less extensively studied than scheduled waking, demonstrates promise in some cases. Hypnotic suggestion—typically that the individual will awaken if their feet touch the ground—can be implemented through recorded sessions requiring daily practice for 2-3 weeks. The approach carries minimal adverse effects and may benefit individuals unresponsive to or unsuitable for scheduled waking.
Stress Management and Psychological Support
Given the strong association between psychological stress and sleepwalking, addressing underlying anxiety, depression, or trauma through appropriate therapeutic interventions may reduce episode frequency. Cognitive-behavioural therapy, particularly CBT for insomnia (CBT-I), improves overall sleep quality and may indirectly benefit sleepwalking.
Specialist Consultation
Persistent, dangerous, or distressing sleepwalking warrants consultation with sleep medicine specialists. Complex cases may require comprehensive evaluation including polysomnography, neurological assessment, or psychiatric evaluation depending on presentation and associated features.
Special Considerations for Different Populations
For children, reassurance often suffices given the typical trajectory toward spontaneous resolution during adolescence. Scheduled waking proves particularly effective and safe. Parents should guide wandering children gently back to bed rather than attempting aggressive interventions or shouting.
For adults, particularly those with new-onset sleepwalking, comprehensive evaluation becomes essential to exclude secondary causes including neurological conditions or substance effects. Addressing comorbid medical and psychiatric conditions, optimising sleep quality, and implementing safety measures take precedence.
The Prognosis: What Does the Future Hold?
The long-term outlook for somnambulism varies substantially based on age of onset and associated factors.
Childhood-Onset Sleepwalking
Children with somnambulism typically enjoy excellent prognosis. Approximately 99% of children who sleepwalk cease having episodes by adulthood, with most improvement occurring as individuals reach puberty and adolescence. This spontaneous resolution correlates with developmental changes including decreased proportion of slow-wave sleep and central nervous system maturation.
However, persistence beyond adolescence suggests greater likelihood of continuation into adulthood, with at least 25% of children with recurrent sleepwalking potentially continuing to experience episodes.
Adult Sleepwalking
Adult presentations follow more variable courses. Over 80% of adult sleepwalkers report episodes lasting five or more years, indicating the condition’s chronic nature in this population. Unlike childhood-onset cases, adult sleepwalking less frequently resolves spontaneously, though episode frequency often diminishes over time.
Overall Outlook
For the vast majority of affected individuals, somnambulism does not indicate serious underlying pathology. With appropriate safety precautions and management strategies where indicated, most people with sleepwalking lead entirely normal lives. The key lies in realistic expectations, appropriate assessment, and tailored interventions matching individual circumstances.
Advancing Understanding and Embracing Comprehensive Care
Somnambulism exemplifies the complexity of sleep disorders—conditions situated at the fascinating intersection of neuroscience, genetics, development, and environment. Far from being merely an amusing curiosity, sleepwalking represents a legitimate medical condition deserving serious attention, particularly when episodes cause distress, danger, or disruption.
The past decades have witnessed substantial advances in understanding this ancient phenomenon. Genetic research has illuminated hereditary patterns, neuroimaging has revealed the paradoxical brain states underlying episodes, and epidemiological studies have clarified prevalence across populations and age groups. Yet significant knowledge gaps remain, particularly regarding precise mechanisms and optimal management strategies.
The Australian healthcare landscape, with its emphasis on integrated, evidence-based care, positions practitioners to deliver comprehensive assessment and management of sleep disorders including somnambulism. The recognition of sleep health as a national priority in 2023 reflects growing appreciation for sleep’s fundamental role in overall wellbeing.
For individuals and families navigating somnambulism, knowledge proves empowering. Understanding that episodes emerge from deep sleep rather than dream states, recognising the strong genetic component, appreciating the typical trajectory toward resolution in childhood cases, and implementing evidence-based safety measures and behavioural interventions all contribute to reduced anxiety and improved outcomes.
The condition reminds us that consciousness exists not as a binary state but as a spectrum—that the boundaries between sleep and wakefulness prove more permeable than everyday experience suggests. As research continues illuminating the neural mechanisms underlying parasomnias, we move closer to comprehensive understanding and increasingly targeted interventions.
Is sleepwalking dangerous, and should I wake someone who is sleepwalking?
Sleepwalking carries potential injury risk from falls, collisions, or other accidents during episodes. Contrary to popular myth, you can wake a sleepwalker without causing harm, though they will likely experience several minutes of confusion and disorientation. The safest approach involves gently guiding the person back to bed without startling them. Implementing comprehensive safety measures—securing windows and doors, removing hazards, installing stair gates—proves more critical than attempting to prevent specific episodes.
Will my child outgrow sleepwalking, or does it indicate a serious problem?
Approximately 99% of children who sleepwalk cease having episodes by adulthood, with most improvement occurring during adolescence as slow-wave sleep decreases and brain maturation progresses. Childhood sleepwalking typically does not indicate serious underlying pathology, particularly when family history exists and development proceeds normally. However, episodes causing significant distress, danger, or daytime impairment warrant professional evaluation.
What causes sleepwalking, and why does it run in families?
Genetic predisposition represents the most well-established cause of sleepwalking. Children with one affected parent face a 47% risk of developing the condition, which escalates to 61% if both parents are affected. Specific gene variants, including HLA-DQB1*05 and loci on chromosomes 20 and 18, have been identified. Beyond genetics, sleep deprivation, stress, irregular sleep schedules, fever, and comorbid sleep disorders can all trigger episodes in susceptible individuals.
How is sleepwalking diagnosed, and do I need a sleep study?
Diagnosis relies primarily on a detailed clinical history, including witness reports and possibly home video recordings. Polysomnography (sleep study) is considered the gold standard when episodes occur during monitoring, but is rarely needed for straightforward cases. Sleep studies are typically reserved for adult-onset cases, when dangerous behaviors are present, or if there is diagnostic uncertainty.
What can be done to prevent or manage sleepwalking episodes?
Management centers on safety measures such as securing the environment, removing potential hazards, and using alarms. Scheduled waking—waking the individual 15-30 minutes before the typical episode time—has proven effective. Additionally, optimizing sleep hygiene, addressing underlying conditions like sleep apnea, and stress management can help reduce the frequency and severity of episodes. In persistent or dangerous cases, specialist consultation is recommended.