Picture this: you’re walking alone at dusk when a sudden noise startles you from behind. In an instant, your heart pounds, your muscles tense, and your senses sharpen. This isn’t conscious thought—it’s your body’s ancient survival mechanism activating in milliseconds. That same biological response that once saved our ancestors from predators now activates dozens of times daily in response to work deadlines, traffic jams, and smartphone notifications. Understanding adrenaline—the hormone orchestrating this remarkable cascade—reveals why our evolutionary gift has become a modern health challenge, affecting cardiovascular function, mental wellbeing, and metabolic health in ways our ancestors never experienced.
What Exactly Is Adrenaline and How Does It Function in the Body?
Adrenaline, known scientifically as epinephrine, represents one of nature’s most sophisticated chemical messengers. Produced primarily by the adrenal glands—small, hat-shaped endocrine organs perched atop each kidney—this catecholamine functions simultaneously as both a hormone and a neurotransmitter. The adrenal medulla, the inner portion of these glands, synthesises adrenaline from its biochemical precursor, norepinephrine, through a precisely regulated enzymatic process.
What distinguishes adrenaline from other hormones is its remarkable versatility in communication. Once released into the bloodstream, adrenaline molecules circulate throughout the body, binding to specialised adrenergic receptors embedded in cellular membranes across virtually all tissues. These receptors—classified into five subtypes (α-1, α-2, β-1, β-2, and β-3)—trigger different physiological responses depending on their location and expression patterns. A single adrenaline molecule binding to β-2 receptors in bronchial tissue dilates airways, whilst that same molecule binding to β-1 receptors in cardiac tissue accelerates heart rate.
This universal receptor distribution explains adrenaline’s extraordinary power to coordinate whole-body responses within seconds. The hormone’s effects manifest within minutes of release, demonstrating the exquisite efficiency of this ancient survival system. In Australia and New Zealand, the term “adrenaline” predominates in both clinical and colloquial usage, though “epinephrine” remains standard nomenclature elsewhere globally.
The synthesis pathway itself reveals nature’s economy. The adrenal glands convert the amino acid tyrosine through a series of enzymatic steps—first to dopamine, then to norepinephrine, and finally to adrenaline through the action of the enzyme phenylethanolamine N-methyltransferase. This final conversion occurs exclusively in the adrenal medulla and specific neurons within the central nervous system, making these tissues the body’s sole adrenaline production centres.
How Does the Fight-or-Flight Response Actually Work?
The fight-or-flight response exemplifies biological engineering at its finest, orchestrating survival through split-second coordination between brain and body. This cascade begins not with conscious thought, but with the amygdala—an almond-shaped cluster of nuclei deep within the temporal lobe responsible for processing emotional significance and threat detection.
When sensory information reaches the amygdala—whether visual recognition of danger or auditory detection of an alarming sound—this ancient brain structure instantly evaluates the stimulus’s threat potential. Remarkably, the amygdala can initiate defensive responses before the brain’s visual processing centres fully analyse what the eyes are seeing, enabling humans to react before conscious awareness catches up. This neural shortcut represents millions of years of evolutionary refinement prioritising survival over contemplation.
Upon detecting danger, the amygdala transmits distress signals to the hypothalamus, effectively the brain’s command-and-control centre. The hypothalamus then activates two complementary systems operating on different timescales. The first, the Sympathetic-Adreno-Medullar (SAM) axis, provides immediate response. The hypothalamus sends signals racing through autonomic nerve fibres directly to the adrenal glands, which respond by flooding the bloodstream with adrenaline and noradrenaline within seconds.
This sympathetic nervous system functions analogously to a vehicle’s accelerator pedal, delivering instantaneous energy to respond to perceived dangers. Effects manifest within minutes: heart rate surges, blood pressure climbs, breathing accelerates, and pupils dilate. Blood flow redirects away from digestive organs and skin toward large muscles and the brain, prioritising tissues essential for immediate survival.
The second system, the Hypothalamic-Pituitary-Adrenal (HPA) axis, provides sustained response for prolonged threats. The hypothalamus releases corticotropin-releasing hormone (CRH), which travels to the pituitary gland, triggering secretion of adrenocorticotropic hormone (ACTH). This hormone stimulates the adrenal cortex to produce cortisol, the primary stress hormone, which maintains heightened alertness for hours. Cortisol levels typically peak approximately 15 minutes after stress onset and remain elevated substantially longer than adrenaline’s acute surge.
The resulting physiological transformation is comprehensive and profound. Metabolically, adrenaline triggers glycogenolysis—the breakdown of stored glucose in the liver releasing sugar into the bloodstream for immediate energy. Simultaneously, lipolysis mobilises fat stores, whilst insulin secretion is suppressed to prevent glucose storage. These coordinated metabolic shifts ensure maximum fuel availability for fighting or fleeing.
Neurologically, sensory perception sharpens dramatically. Pupils dilate to admit more light, enhancing visual acuity. Mental alertness intensifies as the brain receives enhanced oxygen and glucose delivery. Remarkably, pain perception decreases through stress-induced analgesia, enabling continued physical activity despite injury—a phenomenon explaining how individuals perform extraordinary feats during emergencies without registering pain until afterwards.
What Are the Key Differences Between Adrenaline and Noradrenaline?
Though chemically similar and functionally related, adrenaline and noradrenaline (norepinephrine) serve distinct roles within the stress response system. Understanding these differences illuminates the body’s sophisticated approach to managing different physiological demands.
| Aspect | Adrenaline (Epinephrine) | Noradrenaline (Norepinephrine) |
|---|---|---|
| Primary Role | Mainly functions as a hormone | Primarily a neurotransmitter; also a hormone |
| Source of Production | Primarily adrenal glands (medulla); small amount in neurons | Primarily nervous system nerve endings; some from adrenal glands |
| Synthesis | Made from norepinephrine | Made from dopamine |
| Target Tissues | Acts on almost all body tissues | Mainly works to increase and maintain blood pressure |
| Release Timing | Released during times of stress | Released continuously |
| Mechanism | Binds to α- and β-adrenergic receptors | Binds to α- and β-adrenergic receptors |
Noradrenaline functions predominantly as the sympathetic nervous system’s primary neurotransmitter, released continuously at nerve endings to maintain baseline vascular tone and blood pressure. Its role is more localised and sustained, providing ongoing regulation rather than emergency surges. Conversely, adrenaline serves as a broadcasted alarm signal, released in dramatic pulses during acute stress to mobilise whole-body resources rapidly.
This functional division creates complementary layers of response. Noradrenaline handles moment-to-moment autonomic regulation—the unconscious adjustments maintaining blood pressure when you stand, for instance. Adrenaline provides the emergency override, capable of dramatically amplifying cardiovascular output, metabolic rate, and cognitive function when circumstances demand maximal performance.
How Long Do Adrenaline’s Effects Last and How Does Recovery Occur?
The temporal dynamics of adrenaline’s action reveal another dimension of this hormone’s sophistication. Whilst the initial surge occurs within seconds, effects typically persist for 20 to 60 minutes depending on the stressor’s intensity and duration. Physical manifestations—trembling, elevated heart rate, pallor, and heightened alertness—may continue for approximately 20 minutes even after the perceived threat dissipates.
Recovery depends critically on the parasympathetic nervous system, which functions as the body’s “brake” to counterbalance the sympathetic “accelerator”. The vagus nerve, comprising approximately 75 per cent of the parasympathetic nervous system, extends from the brainstem through the neck to the chest and abdomen, connecting to the heart, lungs, digestive organs, and other vital systems.
When danger passes, parasympathetic activation releases acetylcholine as its primary neurotransmitter, initiating the “rest-and-digest” response. Heart rate and blood pressure decline, breathing slows and deepens, digestive processes resume, and the body shifts from energy mobilisation to restoration and repair. This opposing system doesn’t merely switch off the alarm; it actively promotes healing, cellular repair, and energy replenishment.
Heart Rate Variability (HRV)—the variation in time intervals between consecutive heartbeats—provides a window into this delicate balance. Higher HRV indicates healthy interplay between sympathetic and parasympathetic branches, reflecting robust stress resilience and autonomic flexibility. Conversely, reduced HRV suggests autonomic rigidity, often associated with chronic stress, cardiovascular disease, and diminished stress-adaptation capacity.
What Happens When Adrenaline Activation Becomes Chronic?
Whilst acute adrenaline surges enhance survival, chronic activation transforms this protective mechanism into a health liability. The distinction between acute and chronic stress responses represents arguably the most significant health challenge facing modern populations, with implications spanning cardiovascular, metabolic, immune, gastrointestinal, and neuropsychiatric domains.
The General Adaptation Syndrome framework, first described by endocrinologist Hans Selye, conceptualises chronic stress progression through three stages. The alarm reaction stage features initial fight-or-flight symptoms. If stress persists, the resistance stage emerges, characterised by adaptation to elevated stress levels accompanied by poor concentration, irritability, and frustration. Finally, continued stressor exposure precipitates the exhaustion stage, marked by burnout, fatigue, depression, anxiety, diminished stress tolerance, and immune suppression from prolonged stress hormone elevation.
Cardiovascular consequences of chronic adrenaline activation prove particularly concerning. Persistent surges damage blood vessel endothelium and promote atherosclerotic plaque formation through multiple mechanisms. Elevated adrenaline and cortisol levels induce oxidative stress, endothelial dysfunction, and systemic inflammation—processes directly contributing to arterial damage. Chronic elevation of blood pressure and heart rate significantly increases risk for coronary artery disease, stroke, and hypertension. Individuals with stress-related psychological disorders demonstrate substantially higher cardiovascular disease incidence.
Metabolically, chronic stress drives a constellation of disturbances. Elevated cortisol increases appetite whilst promoting fat accumulation, particularly visceral adipose tissue surrounding organs. Prolonged stress contributes to insulin resistance and type 2 diabetes development through multiple pathways, including chronic inflammation, altered glucose metabolism, and hormonal dysregulation. The metabolic syndrome—clustering of obesity, hypertension, dyslipidaemia, and insulin resistance—shows strong associations with chronic stress exposure.
Immune function suffers profoundly under chronic stress. Sustained cortisol elevation suppresses immune responses by inhibiting pro-inflammatory cytokine production, reducing lymphocyte activity, increasing infection susceptibility, and delaying wound healing. Paradoxically, chronic stress simultaneously promotes systemic inflammation through upregulation of inflammatory mediators including interleukin-1β, interleukin-6, and tumour necrosis factor-α. This dual immunosuppression and inflammation creates conditions favouring autoimmune disease development and exacerbation.
Gastrointestinal manifestations emerge through multiple mechanisms. Catecholamines reduce gut blood flow through vasoconstriction, inhibit gastrointestinal secretions and nutrient absorption, alter gut motility (manifesting as diarrhoea or constipation), increase visceral pain sensitivity contributing to irritable bowel syndrome, and impair the gastrointestinal mucosal barrier’s integrity. Dysregulation of the gut-brain axis—bidirectional communication between the central nervous system and gut microbiota—further exacerbates gastrointestinal disorders under chronic stress.
Central nervous system changes under chronic stress potentially contribute to anxiety, depression, and addiction. Research documents that chronic stress-induced HPA axis dysregulation and cortisol resistance implicate various psychiatric conditions including major depression, post-traumatic stress disorder, generalised anxiety disorder, and panic disorder. Elevated inflammatory cytokines, particularly interleukin-1β, stimulate stress hormone release whilst correlating with depressive symptoms. Evidence suggests chronic stress may contribute to neurodegenerative diseases including Alzheimer’s and Parkinson’s through excessive cortisol production, HPA axis dysregulation, and neuroinflammation.
Musculoskeletal effects manifest through sustained muscle tension and metabolic disturbances. Chronic stress maintains muscles in constant guardedness, contributing to tension headaches, migraines, temporomandibular joint disorders, fibromyalgia, chronic low back pain, and myalgia. Prolonged cortisol elevation causes muscle wasting and decreased bone density by inhibiting osteoblast activity whilst promoting osteoclast function, potentially accelerating osteoporosis development.
How Does Adrenaline Relate to Anxiety and Panic Disorders?
The relationship between adrenaline and anxiety disorders reveals how protective mechanisms can malfunction, triggering alarm responses without genuine threats. Panic attacks occur when the fight-or-flight response activates despite absence of real danger—the body responding to perceived rather than actual threats.
Up to 35 per cent of the Australian population experiences a panic attack at some point in their lives, representing a substantial public health concern. Research demonstrates that during panic attacks, epinephrine secretion increases markedly—studies documenting mean increases of 153 per cent—representing preferential adrenal medullary activation. Individuals with panic disorder exhibit elevated cardiac epinephrine spillover even at rest, possibly reflecting loading of cardiac sympathetic nerve stores from repeated panic-induced adrenaline surges.
Multiple factors can prime inappropriate fight-or-flight activation. Chronic stress causes baseline adrenaline elevation, lowering the threshold for panic response. Acute stress from traumatic events may sensitise the system. Habitual hyperventilation disturbs blood gas balance, triggering compensatory responses that mimic danger signals. Intense physical exercise, illness causing physiological changes, and sudden environmental shifts (overcrowded, hot, stuffy environments) can all precipitate panic episodes in susceptible individuals.
The experience of panic attacks creates a vicious cycle. Anxiety about potential panic attacks can itself trigger the feared response, as catastrophic thoughts and hypervigilance maintain sympathetic activation. This anticipatory anxiety keeps the stress response system primed, paradoxically increasing panic attack frequency.
Effective panic disorder management typically involves cognitive behavioural therapy (CBT), which addresses underlying catastrophic thinking patterns and maladaptive cognitions driving the disorder. Gradual exposure to feared situations, sometimes termed paradoxical intention, helps desensitise the alarm response. Lifestyle modifications including regular exercise, balanced nutrition, yoga, and meditation support autonomic nervous system rebalancing, reducing panic attack frequency and intensity without requiring ongoing intervention.
What Evidence-Based Approaches Help Regulate Adrenaline and Manage Chronic Stress?
Given chronic stress’s pervasive health impacts, evidence-based stress management techniques deserve careful consideration. Research from institutions including Harvard Medical School’s Benson-Henry Institute for Mind Body Medicine demonstrates specific interventions’ effectiveness in countering maladaptive stress responses.
Deep breathing and relaxation response techniques activate the parasympathetic nervous system directly. A double-blind, randomised controlled trial involving 122 patients aged 55 and older with hypertension found that after eight weeks of relaxation response training, 34 or more patients achieved systolic blood pressure reductions exceeding 5 millimetres of mercury, demonstrating significant improvements in blood pressure management through these lifestyle approaches. Techniques eliciting relaxation response include deep abdominal breathing, focus on soothing words, visualisation of tranquil scenes, repetitive prayer, yoga, and tai chi.
Physical exercise provides powerful stress buffering through multiple mechanisms. Research demonstrates that aerobic exercise training significantly increases Heart Rate Variability, indicating improved autonomic nervous system balance. Regular moderate exercise relieves stress-induced cardiovascular response, promotes parasympathetic activity, and prevents cardiovascular disease by adapting baseline cardiac performance. A brisk walk shortly after experiencing stress deepens breathing, relieves muscle tension, and accelerates stress hormone clearance. Movement therapies combining fluid movements with deep breathing—yoga, tai chi, and qi gong—offer particular benefits by engaging both physical and contemplative dimensions.
Mindfulness meditation and yoga interventions effectively reduce sympathetic nervous system activity whilst increasing parasympathetic engagement. A 2016 systematic review in the Journal of Alternative and Complementary Medicine documented mindfulness-based interventions’ efficacy in rebalancing autonomic function. These practices encourage observation of thoughts without judgement, reduce sympathetic overactivity, build stress resilience, reduce brain reactivity to stressors, and improve Heart Rate Variability.
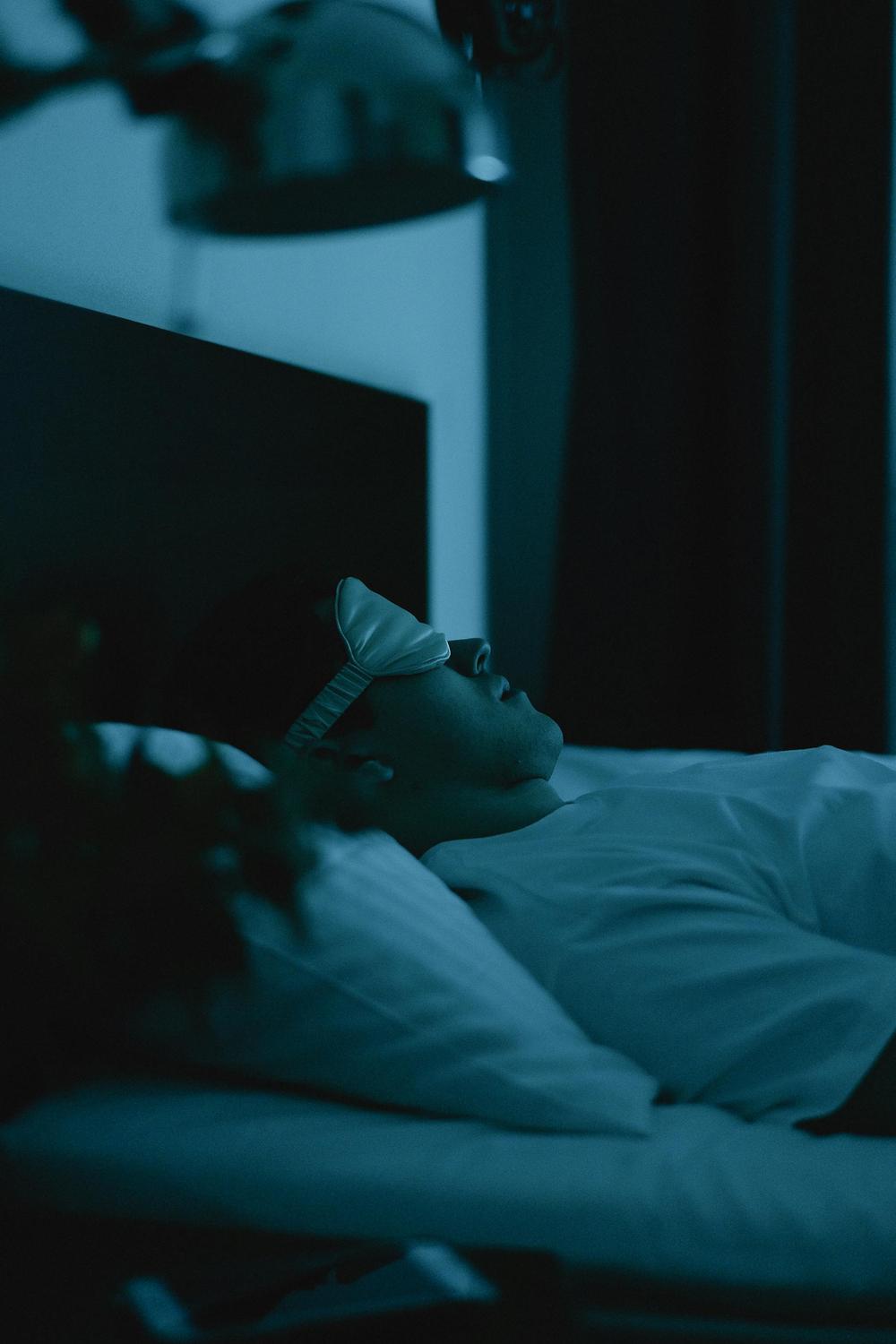
Sleep prioritisation proves foundational for autonomic balance. Adequate, restful sleep—at least eight hours—allows the body to repair and rebalance autonomic function. Sleep deficits cause over-activity in stress response systems, contributing to autonomic dysregulation. Avoiding electronic devices and blue light exposure before bedtime supports sleep quality and proper recovery processes.
Social support provides crucial buffering against chronic stress effects. Healthy relationships and social connections offering emotional support help reduce stress and anxiety, decrease loneliness, support emotional wellbeing, and buffer against chronic stress impacts. Friends, family, and peers who listen empathetically and provide emotional validation represent invaluable resources for maintaining physical and mental health during challenging periods.
Lifestyle modifications including whole-food dietary patterns low in processed and refined carbohydrates, reducing consumption of stimulating beverages, avoiding smoking, and maintaining other healthy habits all support autonomic balance. These lifestyle choices help reduce sympathetic nervous system activation and support cardiovascular health. Cognitive and emotional practices including gratitude journalling, emotional awareness development, progressive muscle relaxation, and grounding techniques complement physiological interventions.
Moving Toward Autonomic Balance in Modern Life
Understanding adrenaline’s dual nature—simultaneously protective and potentially pathological—illuminates a fundamental challenge of modern existence. The same neurochemical cascade that enabled our ancestors’ survival now activates repeatedly in response to psychological stressors lacking physical resolution. Traffic jams, work deadlines, financial concerns, and social media notifications trigger identical hormonal responses as encountering predators, yet without the physical discharge that would naturally complete the stress cycle.
The autonomic nervous system requires balance between sympathetic activation and parasympathetic recovery. When both branches work harmoniously, the body responds appropriately to varying situations—mobilising resources when needed, then fully recovering afterwards. Dysautonomia, reflecting autonomic imbalance, currently affects over 70 million people worldwide, manifesting through blood pressure changes, breathing difficulties, digestive disturbances, heart rate irregularities, and numerous other symptoms.
Recognising that chronic stress represents not weakness but rather a mismatch between ancient biology and modern environment empowers individuals to address this challenge systematically. The evidence-based approaches described—deep breathing, exercise, mindfulness, sleep prioritisation, and social connection—work not by eliminating stress, but by restoring the natural oscillation between activation and recovery that characterises healthy autonomic function.
What triggers adrenaline release in the body?
Adrenaline release begins when the amygdala—the brain’s threat-detection centre—perceives danger or stress. This can include genuine physical threats, psychological stressors such as work pressure or relationship conflicts, intense emotions, sudden environmental changes, or even minor unexpected events in sensitised individuals. The amygdala sends distress signals to the hypothalamus, which activates the sympathetic nervous system and triggers rapid adrenaline secretion from the adrenal glands.
Can you have too much or too little adrenaline naturally?
Whilst having too little adrenaline occurs rarely, excess adrenaline is more common. Chronic stress causes repeated adrenaline surges, potentially leading to persistent elevation that manifests as anxiety, difficulty sleeping, heart palpitations, high blood pressure, weight changes, and an increased risk of cardiovascular disease. Certain rare tumors can also cause pathological adrenaline overproduction.
How can I tell if my adrenaline response is functioning normally?
A healthy adrenaline response activates appropriately during genuine stress—such as during exercise or emergencies—then subsides completely afterwards, allowing full recovery. Warning signs of dysregulation include frequent anxiety or panic attacks without clear triggers, difficulty calming down after stressful events, chronic insomnia despite fatigue, persistent muscle tension, digestive disturbances, and unexplained heart palpitations. Measuring Heart Rate Variability (HRV) can also provide insights into autonomic balance.
What’s the difference between healthy stress and harmful chronic stress?
Healthy stress, or eustress, involves a time-limited activation followed by full recovery. It can enhance cardiovascular performance and cognitive function. Harmful chronic stress, or distress, occurs when stressors persist without adequate recovery, leading to negative health effects such as cardiovascular damage, metabolic dysfunction, immune suppression, and increased risk of anxiety and depression.
Are there natural ways to help balance my stress response system?
Yes, evidence-based techniques such as deep breathing exercises, regular aerobic exercise, mindfulness meditation, prioritising sleep, and maintaining healthy social connections can help rebalance the autonomic nervous system. Lifestyle modifications like eating whole foods, avoiding excessive stimulants, and practices such as yoga or tai chi also support a balanced stress response.