In an era characterised by relentless digital connectivity and accelerating societal demands, millions of Australians find themselves searching for something deeper—a pathway to silence amidst the noise, a method to cultivate presence in a world of perpetual distraction. This universal human longing for connection, meaning, and inner peace has anchored spiritual traditions for millennia through contemplative prayer and meditative religious practices. These ancient disciplines, once confined to monasteries and meditation halls, now stand at a remarkable intersection where faith traditions, neuroscience, and integrative wellness converge with measurable, empirically validated outcomes.
What Is Contemplative Prayer and How Does It Differ from Other Meditation Practices?
Contemplative prayer constitutes a distinctive form of spiritual practice that transcends verbal petition or intellectual analysis, instead emphasising silent, receptive communion with the divine through focused attention and profound presence. The Catholic Catechism describes contemplative prayer as “a simple gaze upon God in silence and love”—a gift characterised by listening rather than speaking, receiving rather than requesting.
This practice carries ancient roots extending to the Desert Fathers of the fifth century, refined through centuries by mystics including St Teresa of Avila, St John of the Cross, and twentieth-century contemplatives like Thomas Merton. Historical descriptions portray contemplation as “a close sharing between friends,” distinguishing it fundamentally from active meditation, which employs thought, imagination, and emotion to deepen faith understanding.
The essential distinction lies in the practitioner’s stance: meditation actively engages mental faculties to reflect upon spiritual truths, whilst contemplation assumes a receptive posture, often described as “resting in God’s presence.” This differentiation proves crucial for understanding research outcomes, as contemplative prayer uniquely combines the psychological mechanisms observed in secular mindfulness with elements of transcendent connection that produce distinct neurological signatures.
Contemporary forms of Christian contemplative practice include Centering Prayer, which employs a sacred word (such as “peace” or “love”) repeated silently for twenty to thirty minutes to consent to divine presence. Lectio Divina offers a four-stage process of reading, meditation, prayer, and contemplation on Scripture. Eastern Orthodox traditions practise Hesychasm, emphasising stillness and silence, whilst the repetitive Jesus Prayer facilitates continuous awareness.
How Do Religious Traditions Practise Contemplative Meditation Across Cultures?
Contemplative practices constitute a genuinely universal human phenomenon, manifesting across every major religious tradition with remarkable consistency in their emphasis on focused attention, present-moment awareness, and cultivation of inner stillness. This universality suggests these practices address fundamental aspects of human consciousness and wellbeing.
Buddhism offers perhaps the most systematised meditation traditions, including Vipassana (insight meditation observing impermanence), Anapanasati (mindfulness of breathing), Metta Bhavana (loving-kindness meditation), and Zen’s Zazen (seated meditation emphasising direct experience). The Buddha’s Noble Eightfold Path includes “right meditation” as essential to spiritual development, positioning contemplative practice as central rather than supplementary.
Hindu traditions developed Dhyana (deep meditation leading toward union with ultimate reality), systematised in Patanjali’s Yoga Sutras as an eight-limb path culminating in meditation and absorption. Mantra repetition of sacred sounds like “Om” combined with Pranayama (breath control techniques) creates comprehensive meditative systems influencing global wellness practices.
Islamic contemplative practices centre on Dhikr—remembrance of God through repetition of divine names and attributes. Sufis developed elaborate practices including Sama (rhythmic chanting), the whirling of Mevlevi dervishes, and Muraqabah (observing one’s thoughts to maintain consciousness of God). The Qur’an explicitly instructs: “O Believers! Remember God with frequent remembrance” (Surah Al-Ahzab 33:41).
Jewish mystical traditions emphasise Kavanah (deep intention transforming routine prayer into profound encounter), Hitbodedut (spontaneous personal meditation in solitude), and Qabbalah’s visualisation practices using the Tree of Life to meditate on divine attributes. Talmudic sources describe rabbis meditating for hours before and after services.
| Religious Tradition | Primary Practice | Core Technique | Duration Focus |
|---|---|---|---|
| Christianity | Centering Prayer, Lectio Divina | Sacred word repetition, Scripture contemplation | 20-30 minutes daily |
| Buddhism | Vipassana, Zazen | Breath awareness, present-moment observation | 10-60 minutes daily |
| Hinduism | Dhyana, Mantra meditation | Sound vibration, breath control | 20-45 minutes daily |
| Islam | Dhikr, Muraqabah | Divine name repetition, self-observation | Multiple daily sessions |
| Judaism | Kavanah, Hitbodedut | Intentional prayer, solitary meditation | Variable, integrated with prayer times |
This cross-cultural consistency reveals contemplative practices address universal aspects of human neurology and consciousness, explaining their persistence across vastly different theological frameworks and cultural contexts.
What Does Neuroscience Reveal About Contemplative Prayer and Brain Function?
Modern neuroimaging technologies have revolutionised our understanding of how contemplative practices physically reshape brain structure and function. These findings elevate meditation from subjective spiritual experience to objectively measurable neurological phenomenon with profound implications for health and wellness.
Structural brain changes (neuroplasticity) represent perhaps the most compelling evidence. Research demonstrates meditation increases cortical thickness in the prefrontal cortex (governing attention, emotional regulation, and decision-making), anterior cingulate cortex (conflict monitoring and attention), and insula (interoception and self-awareness). Gray matter expansion occurs significantly in the hippocampus—the brain region critical for memory and emotional regulation—with greater expansion correlating directly with practice hours.
These changes aren’t subtle. Studies show cortical thickness increases of 0.5 to 1.0 millimetres in prefrontal regions after merely eight weeks of consistent practice. Long-term practitioners with fifteen-plus years of experience display even more pronounced structural modifications, suggesting cumulative neuroplastic benefits.
Functional brain changes prove equally remarkable. Contemplative prayer reduces activity in the Default Mode Network (DMN)—brain regions including the medial prefrontal cortex and posterior cingulate cortex responsible for mind-wandering and rumination. This reduction correlates directly with decreased anxiety and depression, as excessive DMN activity associates with negative thought patterns and self-referential rumination.
Simultaneously, meditation enhances activity in the dorsolateral and ventromedial prefrontal cortex, strengthening executive attention networks that support focused concentration and behavioural regulation. The amygdala—the brain’s threat-detection centre—shows reduced reactivity to emotional stimuli, with this reduction correlating with accumulated meditation hours.
Perhaps most intriguingly, long-term meditators demonstrate sustained high-amplitude gamma synchrony (25-100 Hz oscillations) during practice, indicating heightened consciousness and neural integration across brain regions. This represents a distinct neurological state observable through electroencephalography (EEG).
Neurochemical changes extend these structural and functional modifications. Meditation increases serotonin production supporting mood regulation, enhances GABA levels associated with relaxation, and significantly reduces cortisol—the primary stress hormone. Research demonstrates meditation affects gene expression related to inflammatory response, energy metabolism, and cellular repair, suggesting practices influence health at the most fundamental molecular level.
These findings establish that contemplative prayer and meditative religious practices produce measurable, reproducible changes in brain architecture, chemistry, and function—changes that persist beyond practice sessions and accumulate over time.
How Do Contemplative Practices Support Mental and Physical Wellbeing?
The neurological changes described above translate into substantial, clinically meaningful improvements across multiple dimensions of psychological and physical health, positioning contemplative practices as legitimate, evidence-based wellness interventions.
Psychological and Emotional Benefits
Stress reduction and anxiety management represent the most consistently documented outcomes. Meta-analyses demonstrate mindfulness-based interventions produce small to moderate reductions in stress and anxiety across diverse populations. Centering Prayer research specifically shows participants experience decreased stress and anxiety from baseline to post-intervention, with mechanisms involving parasympathetic nervous system activation (the body’s “rest-and-digest” response) and reduced sympathetic activation.
Regular practitioners display lower baseline cortisol levels and reduced stress hormone response to challenges, indicating improved stress resilience rather than merely temporary relaxation. This reduction in allostatic load—the cumulative physiological wear and tear from chronic stress—proves particularly valuable for long-term health maintenance.
Depression management shows equally promising outcomes. Mindfulness-based interventions demonstrate effectiveness for reducing depressive symptoms and preventing relapse, with contemplative practices associated with faster remission from depression in at-risk populations. The mechanism involves reducing rumination and negative thought patterns whilst increasing perspective-taking capacity—the ability to observe thoughts and emotions without automatic identification or reaction.
Intriguingly, some research suggests religious or spiritual forms of meditation produce superior outcomes for depression compared with secular versions in certain populations, possibly due to enhanced meaning-making and existential support.
Emotional regulation and resilience improve markedly. All groups practising contemplative techniques show increases in positive emotion and decreases in negative emotion. Meditation enhances emotion regulation through strengthened prefrontal-limbic circuits, allowing practitioners to experience emotions fully whilst maintaining equanimity—the capacity to remain calm when facing difficulty.
Research conducted during the COVID-19 pandemic demonstrated older adults with established meditation practices maintained higher resilience during lockdowns and health uncertainties. Self-compassion—protecting against shame and self-judgment—increases significantly following meditation training.
Cognitive benefits extend beyond emotional domains. Practitioners demonstrate improved concentration, sustained attention, and ability to suppress distracting information. Working memory capacity and information retention enhance, whilst cognitive flexibility—the ability to shift perspectives and adapt thinking—improves measurably. Executive function improvements include enhanced impulse control, decision-making, and behavioural flexibility.
Cardiovascular and Physical Health Benefits
The mind-body connection manifests powerfully in cardiovascular outcomes. Meta-analyses demonstrate meditation produces clinically meaningful reductions in both systolic and diastolic blood pressure, with some studies showing reductions of 4.8 to 10.7 millimetres of mercury (mmHg) in systolic pressure—representing significant improvements in cardiovascular health outcomes.
Heart rate and heart rate variability (HRV) improvements indicate enhanced parasympathetic tone and improved cardiac vagal control. Slow-paced contemplative practices at approximately six breaths per minute induce particularly favourable cardiovascular effects through respiratory-cardiac synchronisation.
Large population studies reveal striking long-term outcomes. Analysis of over 61,000 participants in the National Health Interview Survey found those who meditated were 51% as likely as non-meditators to have coronary artery disease. Fifteen-year follow-up studies demonstrate 30% reduction in cardiovascular mortality and 23% reduction in all-cause mortality amongst regular practitioners.
Metabolic benefits include improved insulin sensitivity in patients with coronary artery disease, approximately 10% reduction in fasting serum cholesterol with regular meditation, and favourable trends across multiple metabolic syndrome indicators. Patients with Type 2 diabetes demonstrate better glycaemic control when incorporating contemplative practices.
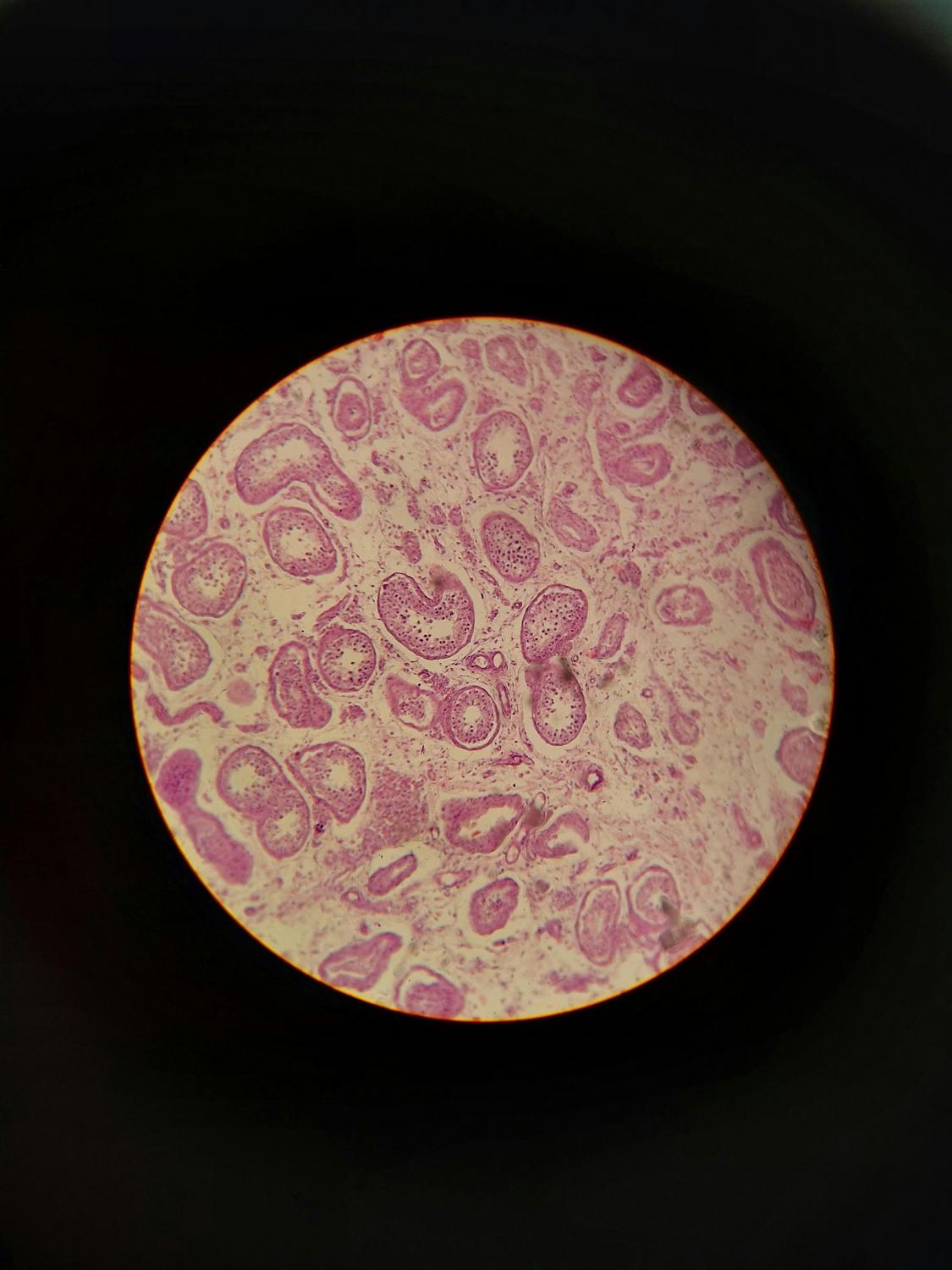
Immune function and inflammation respond positively to regular practice. Studies document increased CD4+ T-cell counts, improved cellular immune response, and enhanced antibody response to vaccination in some meditation practitioners. Pro-inflammatory markers including nuclear factor kappa B, interleukin-6 (IL-6), and tumour necrosis factor-alpha (TNF-α) decrease significantly, whilst C-reactive protein (CRP)—a key inflammation marker—reduces in both meditation and spiritual practices.
These inflammatory reductions prove particularly valuable for conditions with inflammatory components, including cardiovascular disease, autoimmune conditions, and chronic pain syndromes.
What Makes Religious Meditation Different from Secular Mindfulness in Practice and Outcomes?
The relationship between explicitly religious contemplative practices and secular mindfulness approaches represents a nuanced area revealing both similarities and meaningful distinctions with implications for personalised wellness approaches.
A landmark randomised controlled trial conducted at Johns Hopkins University examined 702 Christians across three conditions: Centering Prayer with religious framing, neutral Centering Practice, and passive control. The findings illuminate the complex interplay between religious context and outcomes.
Spiritual and transcendent experiences showed clear differentiation. The religious contemplative prayer group demonstrated significantly higher scores on the Mystical Experience Questionnaire and Daily Spiritual Experience Scale compared with neutral framing. Only the explicitly religious group showed significant increases in awe experiences—moments of wonder and connection with something greater than oneself that research associates with enhanced prosocial behaviour and wellbeing.
However, general psychological wellbeing showed more mixed results. The study found no significant between-group differences on the primary flourishing measure, suggesting religious framing doesn’t necessarily enhance general wellbeing beyond what secular approaches provide. All groups, including neutral practice, showed increased wellbeing from baseline.
Other research reveals contexts where religious framing produces superior outcomes. Studies on pain tolerance demonstrate religious meditation enhances behavioural pain tolerance compared with secular approaches. Research on migraines shows Christian-specific meditation produces the largest reductions in migraine symptoms and frequency among contemplative approaches. For individuals with strong faith commitments, integration of religion appears essential for optimal engagement and outcomes.
The principle emerging from this evidence: contemplative practices work through universal neurological mechanisms affecting attention, emotion regulation, and stress response. Religious framing adds a transcendent dimension providing additional meaning, purpose, and spiritual connection for those to whom such frameworks resonate. Secular approaches access the same neurological pathways whilst remaining accessible to those without religious affiliation.
This understanding supports personalised approaches where practice selection aligns with individual values, beliefs, and cultural background. Australian healthcare contexts—characterised by religious diversity and substantial secular populations—benefit from offering both religiously integrated and neutral contemplative options, allowing individuals to access evidence-based benefits through personally meaningful frameworks.
Integrating Contemplative Practices Within Holistic Wellness Approaches
The convergence of ancient contemplative wisdom with modern neuroscience positions these practices uniquely within comprehensive, person-centred wellness frameworks. Rather than competing with conventional healthcare, contemplative prayer and meditative religious practices offer complementary approaches addressing dimensions of human wellbeing that purely biomedical models cannot fully encompass.
Australian health authorities including healthdirect.gov.au and Beyond Blue increasingly recognise mindfulness and meditation for stress reduction, anxiety management, sleep improvement, and chronic illness support. Medicare Mental Health provisions support access to practitioners trained in mindfulness interventions, reflecting growing integration within mainstream healthcare systems.
The accessibility factor proves particularly significant. Contemplative practices require no equipment, carry minimal to no cost, and can be adapted to culturally meaningful frameworks—making them exceptionally valuable for addressing health disparities and reaching underserved populations. Approximately 8% of Australian adults currently practise some form of meditation, a figure steadily increasing as evidence accumulates and awareness grows.
Implementation success depends on several factors: qualified instruction significantly improves outcomes compared with self-directed approaches; both group and individual formats prove effective, with groups offering additional social support; daily practice—even brief sessions of 5-10 minutes—produces more consistent benefits than sporadic longer sessions; and practices should be tailored to individual preferences, beliefs, and life circumstances.
The “deep rest” model explains mechanistically how contemplative practices work: focused attention and slowed breathing communicate bodily safety, shifting physiology from threat response to rest state. This parasympathetic activation redirects cellular resources from stress mobilisation toward restoration, repair, and optimisation—affecting gene expression, immune function, inflammation, and cellular aging.
Safety considerations remain important. Whilst generally safe with minimal adverse effects when practised appropriately, individuals with psychosis should consult mental health professionals before intensive meditation. Those with trauma histories may require guided practice or combination with therapy. Temporary increases in anxiety occasionally occur as suppressed emotions surface, though qualified instruction and gradual progression minimise such risks.
The research landscape, whilst substantial and growing, acknowledges limitations including small sample sizes in some studies, difficulty measuring adherence in self-directed interventions, and publication bias favouring positive findings. Long-term outcome data beyond 6-12 months remains limited, and optimal dose-response relationships for specific conditions require further clarification.
Nevertheless, the existing evidence base—spanning thousands of peer-reviewed studies across neuroscience, psychology, cardiology, and immunology—establishes contemplative prayer and meditative religious practices as legitimate, evidence-based wellness interventions. These practices don’t replace conventional medical care but enhance it, offering individuals active roles in their health management through accessible, safe, sustainable approaches aligned with their deepest values.
For healthcare consultancies developing sophisticated, holistic wellness frameworks, contemplative practices represent essential components bridging mental, physical, and spiritual dimensions of health. As Australian society continues evolving toward more integrative, person-centred healthcare models, ancient contemplative wisdom validated by modern science offers pathways to resilience, balance, and flourishing available to all, regardless of religious affiliation or socioeconomic status.
Looking to discuss your health options? Speak to us and see if you’re eligible today.
How long does one need to practise contemplative prayer before experiencing benefits?
Research demonstrates measurable benefits can emerge relatively quickly with consistent practice. Studies show neurological changes, including increased cortical thickness and altered brain function, after eight weeks of daily practice. Psychological benefits such as reduced stress and improved mood often appear within four to six weeks. However, the relationship between practice duration and benefits follows a dose-response pattern—more hours of accumulated practice correlate with larger, more stable effects. Even brief daily sessions of 5-10 minutes produce meaningful outcomes, though 20-30 minute sessions show the most consistent results across research. Long-term practitioners with fifteen-plus years of experience demonstrate the most pronounced brain changes and wellbeing outcomes, suggesting benefits continue deepening over time.
Can secular Australians benefit from contemplative practices without religious belief?
Absolutely. Whilst contemplative prayer originated within religious contexts, the underlying neurological mechanisms—including attention regulation, emotional processing, and stress response modulation—function independently of theological belief. Secular mindfulness meditation, which removes religious framing whilst maintaining core contemplative elements, demonstrates equivalent benefits for stress reduction, anxiety management, cardiovascular health, and cognitive function. Research comparing religious and secular approaches shows both produce significant improvements across most health measures. The key distinction lies in spiritual experiences: explicitly religious framing enhances mystical experiences, awe, and existential meaning for those with faith commitments, whilst secular approaches remain equally accessible and effective for those without religious affiliation.
Are contemplative practices safe for individuals managing mental health conditions?
For most individuals, contemplative practices prove safe and beneficial as complementary support for mental health conditions including anxiety, depression, and post-traumatic stress. Research demonstrates effectiveness particularly for anxiety disorders and depression, with mindfulness-based cognitive therapy recognised as evidence-based relapse prevention for depression. However, certain populations should exercise caution: individuals with active psychosis should consult mental health professionals before intensive meditation, those with trauma histories may require trauma-informed, guided approaches, and some individuals with severe anxiety might temporarily experience increased anxiety as suppressed emotions surface. These risks are minimised with qualified instruction, gradual progression, and integration with professional mental health support.
What specific type of contemplative practice works best for cardiovascular health?
Research demonstrates multiple contemplative approaches produce cardiovascular benefits, though practices emphasising slow, rhythmic breathing—around six breaths per minute—tend to induce particularly favourable effects through respiratory-cardiac synchronisation. For example, Transcendental Meditation has been shown to reduce systolic blood pressure by approximately 10.7 mmHg and diastolic pressure by 6.4 mmHg, while mindfulness-based interventions produce moderate reductions. Loving-kindness meditation also shows improvements in heart rate variability. Ultimately, the optimal approach depends on individual preference and adherence, as consistency in daily practice typically produces superior long-term cardiovascular outcomes.
How do contemplative practices fit within comprehensive, integrative wellness approaches?
Contemplative practices are foundational elements within comprehensive wellness frameworks, addressing mental, emotional, and stress-related dimensions that significantly influence physical health. Rather than serving as standalone interventions, they complement other evidence-based strategies such as balanced nutrition, regular physical activity, adequate sleep, and social connection. The stress reduction and emotional regulation achieved through contemplative practices enhance an individual’s capacity to maintain these healthy behaviours, creating a synergistic effect. Within Australia’s evolving integrative healthcare landscape, these practices offer cost-effective, accessible, and culturally adaptable options that empower individuals to take an active role in their overall wellbeing.